The COVID-19 pandemic has posed unprecedented challenges, prompting a critical inquiry: Might our genetic makeup hold the key to more effective treatments in future health crises?
The pandemic has revolutionized healthcare, underscoring the pivotal role of pharmacogenomics in fortifying our defenses against future pandemics. This field, which examines the genetic influence on drug responses, harbors vast potential for tailoring treatments to individual genetic profiles. Insights from COVID-19 are instrumental in refining our approach to future health emergencies through personalized medicine.
The significance of genetic factors in determining drug efficacy and safety has been starkly highlighted. The Centers for Medicare & Medicaid Services (CMS) issued a Local Coverage Determination (LCD) for Molecular Diagnostic Services Program (MoIDX): Pharmacogenomics Testing in June 2020, facilitating wider access to these pivotal tests1. With pharmacogenomic testing gaining broad coverage from July 2020, we are on the cusp of an era where personalized medicine could become the norm in combating infectious diseases.
The integration of pharmacogenomics into pandemic management is both timely and essential, aligning with efforts to enhance drug therapies and reduce adverse reactions2. By deciphering genetic variations, we can tailor treatment plans that account for the diverse genetic makeup of patients. This approach promises to be transformative, ensuring a more resilient public health framework as we move forward. Let’s talk about Lessons from COVID-19: Pharmacogenomics in Preparing for Future Pandemics.

The Impact of COVID-19 on Global Health Systems
The COVID-19 pandemic has unveiled profound impact on global health systems, revealing critical weaknesses in healthcare infrastructures worldwide. By December 3, 2021, the global tally of confirmed cases exceeded 263 million, with fatalities surpassing 5.2 million, underscoring the imperative for an effective pandemic response3. Hospitals were inundated with patients, facing severe shortages of vital medical supplies. This crisis necessitated a reevaluation of healthcare practices, prompting rapid adaptations in many countries to address unprecedented demands.
Under the strain of COVID-19, the significance of efficient treatment methodologies emerged prominently. A 2020 study in JAMA analyzed a broad spectrum of pharmacologic treatments for the virus, emphasizing the critical need for ongoing research and development4. Furthermore, Nature Reviews Drug Discovery underscored the necessity for diverse therapeutic approaches, highlighting the healthcare crisis’s demand for innovation and flexibility in treatment options4.
Research indicated that medications like chloroquine and hydroxychloroquine were considered potential treatments during the pandemic. Studies suggested that hydroxychloroquine could impede SARS-CoV-2 infection in vitro, prompting its evaluation in clinical settings4. However, as these trials progressed, the complexities surrounding drug efficacy and safety emerged, underscoring the requirement for a systematic approach to pharmaceutical therapies in managing COVID-19.
The pandemic served as a catalyst for health policy reform. Governments acknowledged the imperative for comprehensive pandemic preparedness frameworks that encompass both healthcare delivery and research needs. The insights derived from evaluating pharmacological therapies and the performance of global health systems during the COVID-19 impact must inform future strategies to enhance resilience against similar crises.
| COVID-19 Statistics | Data |
|---|---|
| Confirmed cases (as of December 3, 2021) | Over 263 million |
| Total deaths worldwide | Over 5.2 million |
| Genomic sequence identity with SARS-CoV | Approximately 79% |
| Genomic sequence identity with MERS-CoV | Around 50% |
| Genome size of SARS-CoV-2 | Approximately 29.9 kb |
Understanding Pharmacogenomics
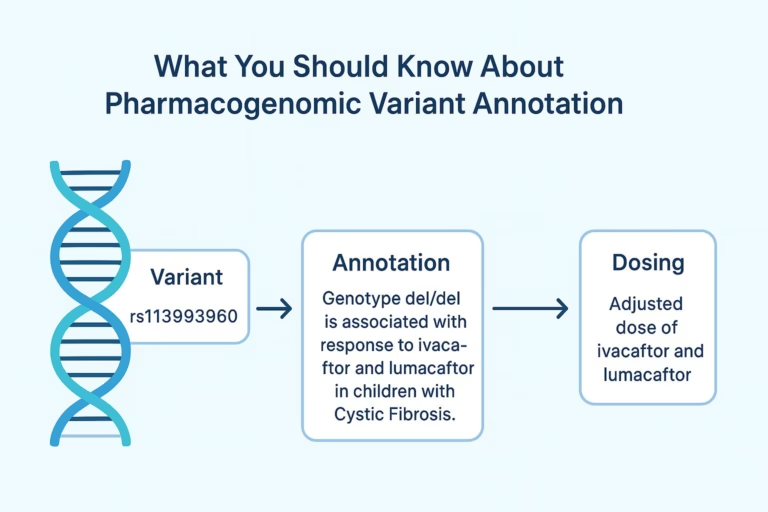
Pharmacogenomics is a discipline that harmonizes pharmacology and genomics to elucidate how genetic variations modulate drug response variability. This field scrutinizes genetic data to tailor medicine to individual genetic profiles, recognizing that genetic heterogeneity across populations significantly influences drug metabolism and efficacy. Hence, genetic testing emerges as crucial for enhancing therapeutic outcomes.
The exploration of cytochrome P450 enzymes, with their polymorphic variants, is pivotal in pharmacogenomics. These variants can substantially affect the efficacy and safety of medications. Research has identified a robust link between genetic markers and the therapeutic efficacy of drugs in COVID-19 treatment, highlighting pharmacogenomics’ significance in managing infectious diseases. This knowledge facilitates a paradigm shift towards personalized medicine, where treatment strategies are customized according to genetic profiles.
Recent investigations have revealed adverse effects in patients administered chloroquine and hydroxychloroquine, medications once hailed for their antiviral efficacy. Scrutiny of their safety in diverse populations has intensified. Pharmacogenomics offers vital insights to avert potential complications from these therapies, thereby augmenting patient safety and treatment efficacy in infectious disease management5.
The progression of pharmacogenomics necessitates the integration of pharmacogenetic tests into routine clinical practices, thereby optimizing drug efficacy and diminishing adverse reactions. This understanding empowers healthcare professionals to formulate more efficacious treatment plans, thus propelling the healthcare delivery landscape forward.
Pharmacogenomics in Preparing for Future Pandemics
As we confront the specter of future pandemics, the integration of pharmacogenomics within public health frameworks emerges as crucial. This discipline, tracing its roots back to the 1950s, has since evolved to dissect the intricate relationship between genetic makeup and drug efficacy6. Such insights are indispensable for tailoring treatments to individual patients, thereby amplifying the effectiveness of medications amidst health crises.
However, the global adoption of pharmacogenomic testing encounters several hurdles, including the knowledge gap among healthcare providers, the scarcity of conclusive evidence, and reimbursement hurdles6. Overcoming these challenges is essential for bolstering pandemic readiness. The acknowledgment by the American Society of Health-System Pharmacists of pharmacists’ pivotal role in pharmacogenomic testing underscores the potential for community pharmacists to significantly contribute to patient care6.
Pharmacists are indispensable in the dissemination of pharmacogenomic testing, spanning from outpatient clinics to community pharmacies6. Their proactive involvement in medication management can significantly benefit patients, especially in chronic disease management and medication use during outbreaks6.
The incorporation of pharmacogenomics not only enhances patient outcomes but also empowers patients to take a more active role in their healthcare. For instance, the use of polygenic risk scores can precipitate behavioral changes, such as increased patient engagement with healthcare providers and lifestyle enhancements7. Moreover, pharmacogenomics can significantly refine chemotherapy protocols, ensuring their efficacy while minimizing adverse effects7.
In conclusion, the strategic deployment of pharmacogenomics can revolutionize our approach to pandemics by enabling personalized treatment strategies. This, in turn, will significantly enhance the efficacy of medications and bolster public health outcomes.
The Role of Genetic Variations in Drug Response
Genetic variations significantly shape individual responses to medications, influencing treatment efficacy. Recognizing these variations is pivotal for tailoring medications to a patient’s genetic profile. Genes such as CYP2D6 and CYP2C9, crucial for drug metabolism, play significant roles in determining therapeutic outcomes.
Pharmacogenetic testing emerges as a critical tool in clinical environments, predicting patient responses to various drugs, including those for cancer and blood thinning. Genetic analysis can prevent most Adverse Drug Reactions (ADRs), which are the fourth leading cause of death in the U.S., resulting in around 100,000 fatalities annually8. Genetic differences can disrupt metabolic pathways, leading to both common and severe ADRs8.
The concept of personalized medicine gains importance during pandemics, where drug efficacy can differ significantly across populations. This highlights the need for tailored treatment plans informed by pharmacogenetic insights9. However, the integration of pharmacogenomics in clinical settings is hindered by several challenges, including the high cost of genetic testing due to limited insurance coverage and substantial out-of-pocket expenses for patients8.
Access to genetic expertise and resources also poses practical obstacles, leading to delays as samples may need to be sent out for testing. Additionally, public unfamiliarity with pharmacogenomics hampers its wider adoption in healthcare. For deeper insights into pharmacogenomics, resources such as the RACGP guidelines on pharmacogenomics offer valuable information.
The Importance of Personalized Medicine During Outbreaks
The COVID-19 pandemic has highlighted the pivotal role of personalized medicine in managing outbreaks. By tailoring treatments to an individual’s genetic makeup, the effectiveness of therapies during pandemics can be significantly enhanced. For example, a study in Spain revealed that COVID-19 patients were 4.75 times more likely to experience severe adverse drug reactions (ADRs) than those without the virus10. This stark contrast underscores the necessity of incorporating pharmacogenomic data into treatment plans.
Adverse reactions complicate treatment strategies, emphasizing the importance of personalized approaches. Genetic variations affecting the pharmacokinetics and pharmacodynamics of COVID-19 medications are still under-studied, highlighting a lack of pharmacogenomic data in current literature10. With over 223 million confirmed cases worldwide by September 202110, the imperative for tailored treatment regimens is clear to reduce risks and enhance patient outcomes.
The integration of personalized medicine with technology, particularly artificial intelligence, heralds a transformative potential for managing outbreaks. The effective use of individualized therapies can fortify healthcare systems against current and future health crises. This is evident in AI applications during the COVID-19 era, setting the stage for significant advancements in therapy design and administration11.
Personalized medicine not only enhances therapeutic outcomes but also tackles the unique challenges posed by outbreaks. The COVID-19 pandemic has taught us the value of prioritizing personalized strategies in public health initiatives. This ensures better preparedness and response in future health emergencies.
Benefits of Genomic Testing in Patient Care
Genomic testing revolutionizes patient care by providing bespoke solutions that significantly boost drug efficacy and safety. It enables healthcare professionals to discern genetic variations that dictate individual responses to medications. This knowledge facilitates the implementation of precision medicine, tailoring treatments to align with the patient’s genomic profile.
Improved Drug Efficacy and Safety
Pharmacogenomics elevates drug efficacy, ensuring that prescribed medications are both effective and safe for patients. Given that nearly 20% of primary care prescriptions are at high risk due to gene variants affecting medication response, genomic testing is crucial12. By integrating genomic insights into treatment strategies, safety and compliance are enhanced, thereby reducing adverse drug reactions. This predictive capability allows healthcare providers to select the most suitable drugs for individuals, thereby improving health outcomes13.
Reduction of Adverse Drug Reactions
Genetic predispositions play a pivotal role in understanding the risk of adverse drug reactions (ADRs), a major concern in contemporary healthcare. Studies show that informing patients about pharmacogenomic information can lead to a 50% increase in medication adherence, subsequently decreasing ADRs12. By screening for genetic variants that influence drug response, clinicians can prevent life-threatening reactions, ensuring a patient-centered approach to therapy14. The growing availability of personal genomics tests from companies like 23andMe and Ancestry.com empowers patients with knowledge of their genetic predispositions, aiding healthcare providers in making more informed treatment decisions14.

| Genomic Testing Benefit | Impact on Patient Care |
|---|---|
| Improved Drug Efficacy | Tailored drug selection based on genetic makeup |
| Safety Enhancement | Reduction of adverse drug reactions |
| Increased Compliance | Higher adherence to medication due to informed decisions |
Current Strategies and Challenges in Pandemic Preparedness
The COVID-19 pandemic necessitated a transformation in healthcare strategies, underscoring the imperative for sophisticated systems to monitor and manage outbreaks. Entities across the globe recognized the criticality of pandemic preparedness, advocating for the establishment of comprehensive frameworks for data collection and dissemination. The Rockefeller Foundation spearheaded an initiative, proposing a national system for the tracking of SARS-CoV-2 genomic variants, thereby bolstering pandemic resilience15.
However, the journey towards enhanced pandemic preparedness is fraught with challenges. A recent study underscored the emergence of a novel coronavirus, inducing severe pneumonia, which highlighted the shortcomings of prevailing pandemic preparedness frameworks15. The imperative for real-time surveillance of pathogen evolution has become paramount, with platforms like Nextstrain playing a pivotal role in this endeavor, facilitating an enhanced comprehension of viral mutations during outbreaks15.
Furthermore, the establishment of integrated genomic surveillance networks is deemed essential for the surveillance of viral evolution. Platforms such as GISAID facilitate the expedited dissemination of genomic data, significantly bolstering global pandemic preparedness efforts15. The American Society of Health-System Pharmacists (ASHP) has underscored the pivotal role of pharmacists in augmenting access to healthcare during pandemics, leveraging the PREP Act to administer COVID-19 therapeutics and vaccinations16.
Despite these efforts, significant gaps persist, necessitating targeted interventions. The ASHP has advocated for enhancements to the Strategic National Stockpile, emphasizing the need for heightened transparency and updates on medical supplies to ensure readiness for future pandemics16. Ongoing surveillance and research into the evolution of pathogens are indispensable for the development of efficacious healthcare strategies.
Case Studies: Pharmacogenomic Applications in COVID-19 Treatment
The quest for effective COVID-19 treatment has led to the integration of pharmacogenomic applications, especially in drug repurposing. Chloroquine and hydroxychloroquine have been at the forefront of treatment protocols since the pandemic’s outset. These drugs, initially touted for their potential against SARS-CoV-2, have been subject to intense scrutiny.
Chloroquine and Hydroxychloroquine in Treatment Protocols
Chloroquine and its derivative hydroxychloroquine were lauded for their potential against SARS-CoV-2. Early studies suggested hydroxychloroquine could reduce COVID-19 mortality rates, based on trials involving thousands of patients. A comprehensive clinical trial with 28,759 mild COVID-19 patients indicated reduced hospitalization rates with hydroxychloroquine, sparking optimism about its therapeutic potential17. However, a trial in Brazil with 667 participants found no significant benefits from hydroxychloroquine alone or with azithromycin, casting doubts on its efficacy17. The FDA’s subsequent withdrawal of its emergency use authorization due to cardiac safety concerns further complicated matters17.
Repurposing Existing Drugs Based on Genetic Testing
The concept of drug repurposing emerged as researchers sought existing agents to combat COVID-19. Pharmacogenomic applications have revealed diverse patient responses, with some benefiting from drugs like ivermectin. Genetic profiles have been shown to influence the efficacy of these drugs in alleviating symptoms. Researchers are now delving into the genetic and molecular interactions of these compounds to refine treatment strategies further. This focus on tailored treatments is crucial for improving patient outcomes during the pandemic, with insights from clinical trials guiding healthcare decisions.
| Drug | Outcome | Trial Size | Notes |
|---|---|---|---|
| Hydroxychloroquine | Reduced hospitalization | 28,759 | Initial optimism later contradicted by other trials17 |
| Hydroxychloroquine | No benefit | 667 | Trial in Brazil |
| Hydroxychloroquine | No benefit | 1,438 | Study in New York State |
| Chloroquine | Emergency approval and later withdrawal | N/A | Withdrawn due to safety concerns17 |
Emerging Technologies in Pharmacogenomic Research
Recent advancements in pharmacogenomic research underscore the transformative impact of emerging technologies on genomic medicine. Techniques such as next-generation sequencing and sophisticated bioinformatics tools are pivotal in deepening our comprehension of drug responses. The integration of artificial intelligence (AI) significantly enhances these technologies by simplifying the analysis of vast genetic datasets, thereby leading to more precise therapeutic strategies.
The role of AI is particularly pronounced in the context of the COVID-19 pandemic, where it has been crucial in various strategic domains including triage, diagnosis, risk prediction, and pharmacogenomics18. For instance, AI-powered technologies effectively forecasted the virus’s spread, as seen with Canadian company BlueDot’s system that alerted of risks in Hubei province in December 201918. Such innovations have significantly advanced pharmacogenomic research, offering insights into genetic determinants of COVID-19 susceptibility and treatment responses.
These emerging technologies empower researchers to transcend conventional boundaries. The employment of human organoids as models for disease studies exemplifies this trend19. Grasping genetic variations in drug responses not only bolsters the development of precision medicine but also opens up significant opportunities for pandemic preparedness. Interdisciplinary approaches and automated organoid workflows, in conjunction with AI analyses, foster a fertile ground for innovation in pharmacogenomic applications.
| Technology | Application | Impact |
|---|---|---|
| Next-Generation Sequencing | Genetic profiling of patients | Enhanced personalized treatment strategies |
| AI in Drug Repurposing | Identifying existing drugs for new uses | Speeding up the availability of treatments |
| Automated Organoid Systems | Modeling disease and drug response | Improved accuracy in predictions for patient care |
| Bioinformatics | Data analysis from genomics | Facilitating precision healthcare decisions |
The synergy between innovation and pharmacogenomic research will continue to redefine the landscape of medicine, ushering in more effective interventions for both routine and pandemic scenarios. The ongoing emphasis on emerging technologies underscores the critical need for adaptability in research and treatment methodologies.
The Future of Precision Medicine in Pandemic Response
The advent of precision medicine is set to revolutionize pandemic response strategies, significantly altering future healthcare landscapes. By seamlessly integrating pharmacogenomics, public health officials can craft interventions that are meticulously tailored to individual patient needs. This approach ensures that treatment efficacy is maximized, while minimizing adverse drug reactions.
Moreover, the utilization of big data and digital technologies is paramount in forecasting and managing outbreaks. Precision public health leverages a plethora of data sources to monitor and regulate infectious diseases, underscoring the critical role of sustained surveillance and targeted community initiatives20. Therefore, the imperative for collaboration among researchers, clinicians, and policy-makers is paramount to surmount the hurdles in implementing these avant-garde strategies.
Looking to the horizon, the fusion of pharmacogenomics and precision medicine heralds a future where healthcare systems are more robust. With forthcoming advancements, communities stand to benefit from significantly improved pandemic response capabilities, thereby diminishing morbidity and mortality during health crises21. As we confront the intricacies of emerging infectious diseases, our collective aim remains steadfast: to elevate personalized healthcare from a luxury to a cornerstone of healthcare, even amidst emergencies. For more great article check out our blog.
Source Links
- https://www.ashp.org/advocacy-and-issues/key-issues/other-issues/additional-advocacy-efforts/ashp-issue-brief-cms-releases-a-future-lcd-for-pharmacogenomics-testing?loginreturnUrl=SSOCheckOnly – Issue Brief: CMS Releases a future LCD for Pharmacogenomics Testing
- https://www.cambridge.org/core/journals/cambridge-prisms-precision-medicine/article/maturing-pharmacogenomic-factors-deliver-improvements-and-cost-efficiencies/6054665190DFB15AA797EE47D33B8E3B – Maturing pharmacogenomic factors deliver improvements and cost efficiencies | Cambridge Prisms: Precision Medicine | Cambridge Core
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8894692/ – Role of genomics in combating COVID-19 pandemic
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7710379/ – Pharmacogenomics landscape of COVID-19 therapy response in Serbian population and comparison with worldwide populations
- https://www.nature.com/articles/s41397-021-00209-9 – Pharmacogenomics and COVID-19: clinical implications of human genome interactions with repurposed drugs – The Pharmacogenomics Journal
- https://www.mdpi.com/2226-4787/11/5/144 – The Critical Role of Pharmacists in the Clinical Delivery of Pharmacogenetics in the U.S
- https://www.medtechviews.eu/articles/time-prepare-revolution-predictive-genomics/ – Time to prepare for the revolution in predictive genomics – MedTech Views
- https://pitjournal.unc.edu/2023/01/05/pharmacogenomics-a-review-of-its-objectives-successes-and-limitations/ – Pharmacogenomics: A Review of its Objectives, Successes, and Limitations
- https://link.springer.com/content/pdf/10.1007/978-3-030-74786-2_294-1.pdf?pdf=inline link – Pharmacogenomics in Developing Countries
- https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.835136/full – Frontiers | Pharmacogenetics and Precision Medicine Approaches for the Improvement of COVID-19 Therapies
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7877825/ – Precision Medicine, AI, and the Future of Personalized Health Care
- https://www.ama-assn.org/delivering-care/precision-medicine/how-pharmacogenomics-enables-precision-approach-care – How pharmacogenomics enables precision approach to care
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131666/ – The Evolution of Public Health Genomics: Exploring Its Past, Present, and Future
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6421958/ – Genomic Testing for Human Health and Disease Across the Life Cycle: Applications and Ethical, Legal, and Social Challenges
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8095210/ – Unlocking capacities of viral genomics for the COVID-19 pandemic response
- https://www.ashp.org/Advocacy-and-Issues/Key-Issues/Other-Issues/Additional-Advocacy-Efforts/ASHP-Submits-Comments-to-Senate-HELP-Committee-on-the-PREVENT-Pandemic-Act – ASHP Submits Comments to Senate HELP Committee on the PREVENT Pandemic Act
- https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.704205/full – Frontiers | The Drug Repurposing for COVID-19 Clinical Trials Provide Very Effective Therapeutic Combinations: Lessons Learned From Major Clinical Studies
- https://www.jmir.org/2021/3/e22453/ – Artificial Intelligence–Aided Precision Medicine for COVID-19: Strategic Areas of Research and Development
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9599083/ – Digital Technologies: Advancing Individualized Treatments through Gene and Cell Therapies, Pharmacogenetics, and Disease Detection and Diagnostics
- https://blogs.cdc.gov/genomics/2020/08/17/precision-public-health-3/ – Precision Public Health and the COVID-19 Response | Blogs
- https://www.mdpi.com/2571-5135/9/1/3 – Precision Medicine in Non-Communicable Diseases