Efavirenz has helped millions of people living with HIV achieve viral suppression, especially in countries where access to newer antiretroviral drugs remains limited. It’s affordable, effective, and widely available. But for many, the experience of taking efavirenz has been far from smooth. Some patients report intense nightmares, anxiety, dizziness, confusion, or even hallucinations. Others quietly stop taking their medication altogether—unable to tolerate the side effects, but unsure why it affects them so differently.
Science now has an answer: it could be your genes.
Efavirenz is broken down in the liver by an enzyme called CYP2B6, and this enzyme is coded for by the CYP2B6 gene. People inherit different versions of this gene. Some versions lead to fast drug metabolism, others to slow metabolism. If you are a slow metabolizer, efavirenz can accumulate in your body to toxic levels, increasing the risk of serious side effects.
According to a PharmGKB clinical annotation, individuals with two copies of the CYP2B6*6 variant—common in African populations—are especially vulnerable. These patients have significantly higher plasma concentrations of efavirenz, even at standard doses. In fact, studies show they can have drug levels three to five times higher than individuals with the normal CYP2B6 gene function.
In one pivotal study published in The Journal of Infectious Diseases (PMCID: PMC3522814), researchers found that individuals with the CYP2B6 516G>T variant (which defines the *6 allele) had a significantly greater risk of experiencing central nervous system toxicity. What’s more alarming is that these side effects often show up early in treatment, leading to poor adherence or discontinuation.
A 2013 study in Pharmacogenomics Journal added another layer of insight. It demonstrated that patients with the slow-metabolizer genotype not only suffered more side effects, but also had persistently high efavirenz levels months into treatment. This supports the idea that adjusting the dose based on genotype could reduce toxicity without compromising HIV suppression.
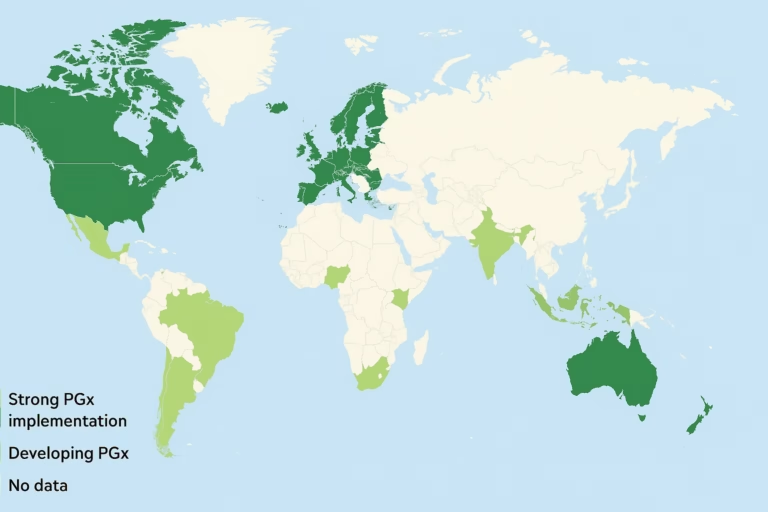
A 2016 systematic review and meta-analysis (PMCID: PMC5612381) examined 27 studies and concluded that CYP2B6 polymorphisms consistently predicted efavirenz plasma concentration and side effect risk. The authors called for the integration of genetic testing into HIV treatment programs, especially in populations with high frequencies of the *6 allele, such as people of sub-Saharan African descent.
Even more striking, a 2016 study from Nigeria showed that nearly 50% of the participants carried the CYP2B6*6 variant, and those individuals had markedly higher rates of neuropsychiatric symptoms. Many of these patients had to switch to alternative regimens, often after weeks or months of distress.
So, what does all this mean for people starting or already on efavirenz?
It means that a simple genetic test could spare many from unnecessary suffering. Testing for CYP2B6 variants can help clinicians decide whether efavirenz is a safe option or whether a lower dose, or a different drug altogether, would be better. In some cases, adjusting the dose from 600mg to 400mg has been shown to reduce side effects in slow metabolizers while maintaining virologic control.
Pharmacogenomic testing isn’t yet standard in most HIV programs, especially in low-resource settings. But that’s beginning to change. As the cost of testing drops and awareness grows, integrating genetics into HIV care is becoming more feasible. For patients, this means better quality of life. For health systems, it means fewer treatment interruptions and better adherence.
Efavirenz remains a valuable option in the global fight against HIV. But it shouldn’t be prescribed blindly. Understanding your CYP2B6 genotype could be the key to making efavirenz work for you.