Despite the rapid evolution of genetic technologies, the integration of genomic insights to alleviate health disparities in underprivileged communities remains a pressing area for further research and application. The high variability in treatment outcomes significantly contributes to the health disparities observed in certain groups, leading to a disproportionate disease burden. While genetics plays a role in disease susceptibility among certain populations, the strategies for leveraging genetic information to optimize disease management differ across populations. Substantial initiatives have been undertaken to showcase the efficacy of pharmacogenomics (PGx) in customizing therapies, yet the exploration of PGx’s role in mitigating health disparities remains underdeveloped. Pharmacogenomics presents a powerful theoretical framework to enhance healthcare delivery; however, it has not been fully embraced as an operational framework to diminish health disparities. Let’s talk about The Role of Pharmacogenomics in Addressing Racial and Ethnic Health Disparities.

The COVID-19 pandemic underscored the potential of preemptive PGx testing, heralding a transition from reactive to preemptive testing1. It has been observed that the majority of genome-wide association studies and clinical trials in pharmacogenomics have focused on individuals of European descent, underscoring a dearth of diversity in genetic and clinical research1. There is a pressing need to enhance the representation of women, particularly those from underserved backgrounds, in pharmacogenomic studies to address sex-specific differences in adverse drug reactions and treatment responses1. Research has underscored the imperative for diversity and inclusion in pharmacogenomic studies, advocating for the diversification of research participants and healthcare settings1.
Introduction to Pharmacogenomics and Health Disparities
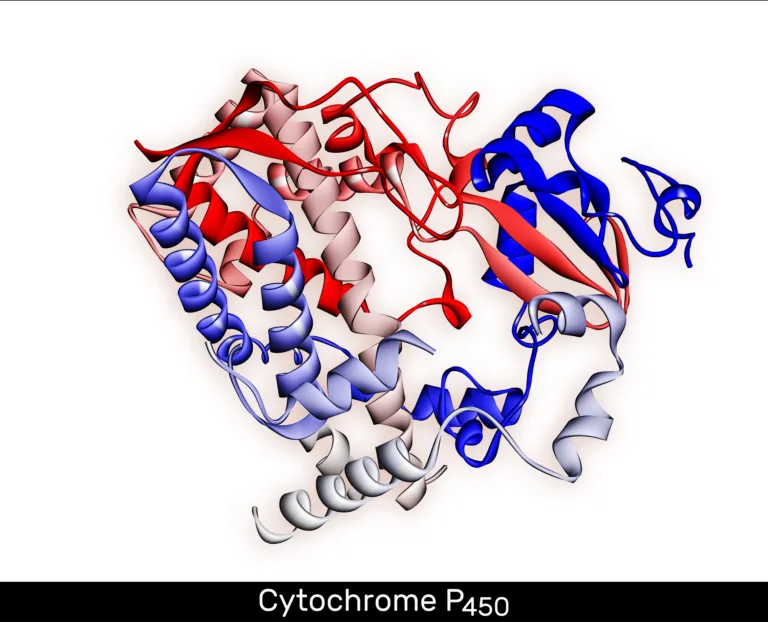
Pharmacogenomics, the discipline examining how genetic makeup affects drug responses, presents a significant opportunity to address health disparities. The disparity in treatment outcomes across diverse populations exacerbates health inequities, leading to a disproportionate disease burden in certain groups2. Identifying genetic determinants of drug efficacy and safety is essential for customizing treatments, especially in minority communities2.
Variability in Treatment Response and Health Disparities
Genetic elements, alongside other risk factors, significantly influence disease susceptibility and treatment efficacy across different racial and ethnic groups2. Research indicates that genetic variants linked to cardiovascular disease exhibit varying frequencies and effects across racial and ethnic demographics2. This disparity in treatment outcomes may underpin the health disparities, where certain populations endure higher morbidity and mortality rates from specific conditions2.
Utility of Pharmacogenomics in Tailoring Therapies
Pharmacogenomics provides a robust framework to enhance healthcare by guiding optimal disease management, enhancing therapeutic outcomes, and reducing adverse drug reactions2. Despite its potential, the integration of pharmacogenomics to address health disparities remains underutilized2. Efforts to harness genetic insights for personalized treatment and outcome enhancement in diverse populations are ongoing, with significant research and implementation underway2.
| Population Group | Cardiovascular Disease Mortality Rate |
|---|---|
| African American Males | 454 per 100,0002 |
| Caucasian Males | 335 per 100,0002 |
| African American Females | 333.6 per 100,0002 |
| Caucasian Females | 238 per 100,0002 |
“Understanding the genetic factors that influence drug efficacy and safety is crucial for tailoring therapies and improving health outcomes, particularly in minority populations.”
Pharmacogenomics in the Post-Pandemic Era
The COVID-19 pandemic has illuminated the pivotal role of pharmacogenomics3 in tackling future health emergencies. The adoption of preemptive pharmacogenomic testing has emerged as a crucial strategy to bolster preparedness and refine patient care3.
Preemptive Pharmacogenomic Testing for Preparedness
Traditionally, pharmacogenomic testing has been reactive, yet the COVID-19 pandemic has showcased the advantages of preemptive testing. By anticipating an individual’s genetic makeup, healthcare professionals can customize treatments effectively, thereby reducing adverse drug reactions, especially in urgent care scenarios3.
Cost-Effectiveness and Outcomes Studies for Implementation
For the widespread acceptance of pharmacogenomic testing, it is imperative to establish its cost-effectiveness and its impact on patient outcomes3. Current research and implementation studies are delving into the benefits of integrating pharmacogenomic data into standard patient care. The goal is to enhance healthcare outcomes and alleviate the strain on healthcare resources3.
In the post-pandemic era, the incorporation of pharmacogenomics into healthcare will be vital for augmenting preparedness and refining treatment strategies3. By harnessing genetic insights, healthcare providers can offer more tailored and efficacious care, thereby addressing health disparities and enhancing patient outcomes3.
Pharmacogenomics and Health Disparities: The Need for Diversity and Inclusion
Precision medicine is poised to revolutionize healthcare by enhancing outcomes for individuals and populations alike. However, the successful implementation of these strategies necessitates a nuanced approach to address health disparities effectively and sustainably4. The integration of pharmacogenomics into healthcare could inadvertently exacerbate health disparities if not executed with a keen awareness of the potential consequences. This includes limiting access to precision medicine for minorities and individuals from lower socioeconomic backgrounds.
The dominance of European ancestry in genome-wide association studies and clinical trials underscores the significant underrepresentation of genetic and clinical diversity45. This dearth of diversity hinders the development of comprehensive and inclusive guidelines, failing to capture the genetic and clinical complexities of diverse populations4.
- Asia and Africa, home to over 77% of the global population, are underrepresented in pharmacogenomics research, particularly outside North America45.
- Hispanics/Latinos, comprising 18.9% of the U.S. populace, face a heightened risk of adverse outcomes post-anticoagulation therapy with Warfarin, underscoring the need for targeted interventions45.
- African Americans, at high risk for Warfarin-related complications, are frequently absent from clinical trials and pharmacogenomics studies, exacerbating health disparities45.
- Non-Hispanic Whites and Asians dominate clinical trials, leading to the oversight of genetic variants specific to African, Hispanic, or Native American populations, potentially affecting drug efficacy in these groups45.
Addressing these disparities necessitates a concerted effort to enhance the representation of underrepresented populations in clinical trials and to adopt genome-wide approaches that reflect the genetic diversity of diverse ancestral backgrounds45.
| Region | Percentage of Pharmacogenomics Research |
|---|---|
| North America | 71% |
| Asia | 18% |
| Other Regions (Africa, Australia, Europe, South America) | 11% |
Gene-based dosing models exhibit enhanced accuracy when corrected for admixture, highlighting the critical importance of population diversity in pharmacogenomics research4. A burgeoning number of studies are now focusing on biogeographically defined populations, particularly those that have been historically underrepresented, such as Native Americans, Africans, and South Asians4.
“Prioritizing the enrollment of participants from less-studied populations in genome-wide association studies (GWAS) and clinical trials is crucial to address health disparities in precision medicine.”
The Role of Pharmacogenomics in Addressing Racial and Ethnic Health Disparities
Pharmacogenomics, the discipline examining how genetic variability affects medication efficacy, is pivotal in mitigating racial and ethnic health disparities. Yet, the dearth of diversity in genetic and clinical research hinders the development of universally applicable guidelines. This scarcity of diversity in research subjects and participants underlines the need for a more inclusive approach to pharmacogenomics.
Lack of Diversity in Genetic and Clinical Studies
Genome-wide association studies and clinical trials predominantly focus on individuals of European descent6. This dominance in research subjects limits our comprehension of genetic influences on treatment efficacy and adverse reactions in diverse racial and ethnic groups. Such a lack of diversity in research perpetuates health disparities, as the derived guidelines and treatment protocols may not be universally effective.
Sex Differences in Adverse Drug Events and Treatment Response
Sex disparities in adverse drug reactions and therapeutic outcomes further complicate health disparities7. Enhancing the representation of women, particularly those from underserved communities, in clinical trials could bridge the sex gap in treatment efficacy and toxicity risks.
To overcome these hurdles, researchers and healthcare professionals must prioritize the inclusion of diverse populations in genetic and clinical studies. Such efforts will not only deepen our understanding of genetic influences on medication response across racial and ethnic groups but also ensure pharmacogenomics benefits are equitably distributed6.
“Advancing diversity, equity, and inclusion in pharmacogenomic research and clinical implementation is crucial to ensuring that the benefits of this transformative field are accessible to all populations, regardless of race, ethnicity, or sex.”
| Characteristic | Percentage |
|---|---|
| Genome-wide association studies with participants of European ancestry | 78% |
| Clinical trials with participants of European ancestry | 81% |
| Clinical trials with female participants | 39% |
Racial, Ethnic, and Genetic Ancestry Diversity in Pharmacogenomic Studies
The realm of pharmacogenomics has emerged as a pivotal approach to address racial and ethnic health disparities. However, the current landscape of pharmacogenomic studies reveals a significant lack of diversity in study populations. Studies have shown profound differences in allele frequencies of genetic variants among socially defined racial and ethnic groups8 and pharmacogenomic variation can predict self-identified race and ethnicity with high accuracy8.
Smoking Cessation and the Need for Diversity
Smoking cessation treatment outcomes vary significantly across racial and ethnic groups, yet the underlying genetic factors driving these differences are not fully understood. Hispanics, African Americans, and individuals of other underrepresented populations remain largely underrepresented in clinical trials and research studies pertaining to pharmacogenomics4. This lack of diversity in study populations limits the ability to develop personalized smoking cessation strategies that address the unique genetic and environmental factors influencing treatment response in diverse communities.
| Population | Representation in Pharmacogenomic Studies | Outcomes in Smoking Cessation |
|---|---|---|
| Non-Hispanic Whites | Overrepresented | Relatively higher success rates |
| African Americans and Hispanics | Underrepresented | Lower success rates and higher relapse rates |
To address this issue, researchers are emphasizing the need for pharmacogenomic studies that reflect the genetic diversity of different ancestral backgrounds.4 Approaches like admixture mapping and the utilization of ancestry-informative pharmacogenetic loci are critical to ensure that the insights gained from pharmacogenomic research can be effectively applied to diverse patient populations4.
“Pharmacogenomic variation predicting self-identified race and ethnicity with high accuracy suggests the need for greater diversity in study populations to ensure the equitable application of personalized medicine.”
By embracing racial, ethnic, and genetic ancestry diversity in pharmacogenomic studies, researchers can unlock the full potential of pharmacogenomics to address disparities in smoking cessation and other areas of healthcare84.
Pharmacogenetic Studies in Geo-Ancestral Population Subgroups
Certain chronic diseases exhibit varying prevalence across populations, mirroring differences in treatment responses. These disparities are influenced by a complex interplay of factors, with population-specific genetic variants playing a pivotal role. The Hmong, an ethnically and demographically distinct Asian subpopulation, has been historically underrepresented in genetic and clinical research. However, engaging this community in research has revealed genetic variants that significantly impact medication efficacy9.
The Hmong Community and Population-Specific Variants
The Hmong, an ethnic minority with roots in Southeast Asia, has been the subject of recent pharmacogenetic studies. These investigations have pinpointed genetic variants within the Hmong that critically affect their response to standard medications9. Such discoveries highlight the necessity of incorporating diverse, underrepresented populations into pharmacogenomic research. This approach is crucial for elucidating the drivers of health disparities and tailoring treatment strategies9.
Research has shown that the Hmong population harbors a higher prevalence of genetic variants linked to drug metabolism and response, notably in the CYP2C19 gene10. These genetic differences can modulate the efficacy and safety of medications such as antidepressants, antiplatelet agents, and proton pump inhibitors10. Recognizing the pharmacogenomic distinctiveness of the Hmong community enables healthcare providers to refine medication dosing and selection. This approach is essential for enhancing treatment outcomes in this underserved group9.
| Pharmacogenetic Associations in the Hmong Community | Relevant Medications |
|---|---|
| Increased frequency of CYP2C19 variants associated with altered drug metabolism | Antidepressants, antiplatelet drugs, proton pump inhibitors |
| Unique genetic variants in other pharmacogenes, such as HLA and TPMT | Immunosuppressants, thiopurine drugs |
Integrating pharmacogenomic data from diverse populations, like the Hmong, is crucial for mitigating the racial and ethnic disparities in healthcare. These insights enable healthcare providers to tailor treatments more precisely, ultimately enhancing health outcomes across the board9.
Pharmacogenomics in Rural Areas: Educational Workforce Training Program
The COVID-19 pandemic underscored the potential of preemptive pharmacogenomics (PGx) testing to revolutionize therapy outcomes and enhance patient care in acute settings1. However, the disparities in pharmacogenetic testing adoption starkly contrast between urban and rural areas111.
Training Pharmacists in Underserved Communities
To bridge this gap, a comprehensive educational framework was devised to bolster the PGx acumen of pharmacists in rural Minnesota or those serving disadvantaged populations1. This initiative targeted pharmacists eager to bolster health equity, span various pharmacy disciplines benefiting from PGx, and lacked prior PGx knowledge or experience1.
Post-program, a significant number of participants expressed their commitment to integrating the learned concepts into their professional practice1. This underscores the pivotal role of educational programs in equipping pharmacists to incorporate pharmacogenomics into their daily routines, especially in underserved areas where tailored medicine access is scarce111.
| Key Findings from Pharmacogenomics Training Program |
|---|
| – 48 key stakeholders were interviewed for a needs assessment on pharmacogenetic testing implementation12 |
| – Positive opinions on using pharmacogenetics to guide therapy were common among participants12 |
| – Concerns included conflicts with reimbursement and test turnaround time12 |
| – Unique concerns for vulnerable, underserved populations included equitable access based on socioeconomic status and cultural sensitivity12 |
| – Participants showed enthusiasm for using telehealth for pharmacogenetic testing implementation in rural communities12 |
Enhancing diversity in genetic and clinical studies is paramount, as the majority of genome-wide association studies and clinical trials have been confined to individuals of European descent, thereby limiting the development of inclusive guidelines111. It is essential to broaden the scope of pharmacogenetic research to encompass a more diverse population, thereby understanding therapy response variability and delivering tailored care to address health disparities effectively111.
The inverse health equity hypothesis posits that populations with elevated socioeconomic status (SES) gain earlier access to advanced technologies like PGx testing, thereby delaying its adoption for those with lower SES who may require it more urgently111. Individuals from medically underserved areas demonstrated a keen interest in pharmacogenetic testing upon comprehension of its benefits, with cost being a major hurdle to its implementation111.
Pharmacogenetic Testing in Medically Underserved Populations
The evolution of pharmacogenomics necessitates a focus on ensuring equitable access to personalized medicine. The inverse health equity hypothesis posits that new technologies, such as pharmacogenetic testing, initially benefit those with higher socioeconomic status. Conversely, medically underserved communities often experience delayed access13.
Perceptions and Attitudes Towards Pharmacogenetic Testing
A recent survey delved into the perceptions and attitudes of patients from medically underserved populations regarding pharmacogenetic testing13. The majority, predominantly Black with some post-high school education and healthcare terminology proficiency, showed moderate to high interest in pharmacogenetic testing under the condition of no cost13. Their motivations included seeking better medication options, understanding medication effects on their bodies, and being aware of potential risks or side effects13.
Cost Concerns and Privacy Issues
The cost of pharmacogenetic testing has emerged as a significant hurdle, especially for underserved populations14. Additionally, concerns about privacy violations, discrimination in employment, and health insurance denial based on genetic information have been voiced by these communities13.
| Key Findings from Pharmacogenomic Studies | Underserved Populations |
|---|---|
| Black patients were less confident about whether their providers made personalized treatment decisions | 14 |
| White patients were more likely to discuss the impact of personal/genetic makeup on medication response with providers | 14 |
| Black patients reported initiating discussions on personal/genetic makeup on medication response much less frequently | 14 |
| Latinos experienced increasing access to individualized medicine based on a matched-cohort study | 14 |
| Blacks were twice as likely as Whites to be unsure about receiving personalized care | 14 |
To overcome these challenges and ensure equitable pharmacogenetic testing access, sustained efforts are imperative. This entails educating and engaging medically underserved communities, addressing cost and privacy concerns15. Innovative approaches to affordability and diversifying pharmacogenomic research to reflect the needs of all populations are also crucial.
“Ensuring equitable access to personalized medicine is crucial, as the implementation of new technologies often initially benefits populations with higher socioeconomic status, while medically underserved communities face delayed access.”
Future Perspectives on Diversity in Pharmacogenomic Research
The future of pharmacogenomics is laden with potential, yet it is contingent upon the resolution of the diversity conundrum in genetic research. Enhancing diversity within pharmacogenomic endeavors will significantly broaden our comprehension of treatment variability, heralding a shift towards bespoke healthcare16.
Engaging Community, Patients, and Providers
Realizing this vision necessitates a collaborative effort to incorporate diverse viewpoints from the community, patients, and healthcare professionals. Through community engagement, researchers can delve deeper into the specific health needs and concerns of marginalized groups16. This will inform research agendas, tackling the health disparities these populations face16. Furthermore, patient engagement will guarantee that pharmacogenetic testing and tailored therapies are both accessible and affordable to diverse populations16. Lastly, provider engagement is indispensable, as healthcare professionals are instrumental in educating patients, interpreting genetic test outcomes, and implementing personalized treatment strategies.
“Improving genetic diversity in pharmacogenomics studies is essential to addressing racial disparities in adverse drug reactions and healthcare outcomes.”
Enhancing diversity and representation within pharmacogenetic research is pivotal for mitigating health disparities and harnessing the full potential of precision health16. A comprehensive strategy that involves various stakeholders will propel the field of pharmacogenomics towards better serving the healthcare needs of diverse populations, regardless of their genetic background or socioeconomic status.

The trajectory of pharmacogenomics is inescapably tied to the pursuit of diversity and inclusivity. By amplifying the voices of underrepresented communities, patients, and healthcare providers, we can unveil novel insights, forge more efficacious treatments, and ensure the equitable distribution of precision medicine’s benefits1615.
Acknowledgments and Author Contributions
The author, YR, extends heartfelt appreciation to the co-editors, authors, and reviewers whose collective efforts made this Research Topic a reality. YR spearheaded the initiative, crafting the proposal and editorial that encapsulate the topic’s essence15.
This endeavor exemplifies the power of collaboration, bringing together researchers and clinicians from varied disciplines. The author recognizes the invaluable contributions of the authors, whose meticulous research and insightful analyses have significantly enhanced the Research Topic’s depth and breadth7.
Furthermore, the author expresses profound gratitude to the peer reviewers for their meticulous evaluation and insightful feedback. Their commitment to maintaining scientific excellence has been pivotal in refining the Research Topic’s content.
Source Links
- https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2023.1233045/full – Frontiers | Editorial: The role of pharmacogenomics in addressing health disparities: the path, the promise, and the barriers
- http://www.nature.com/scitable/topicpage/pharmacogenetics-personalized-medicine-and-race-744 – Pharmacogenetics, personalized medicine, and race
- https://www.nature.com/articles/s41398-021-01600-7 – Barriers to clinical adoption of pharmacogenomic testing in psychiatry: a critical analysis – Translational Psychiatry
- https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2023.1099541/full – Frontiers | Pharmacogenomics and health disparities, are we helping?
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9900000/ – Pharmacogenomics and health disparities, are we helping?
- https://www.kff.org/racial-equity-and-health-policy/issue-brief/use-of-race-in-clinical-diagnosis-and-decision-making-overview-and-implications/ – Use of Race in Clinical Diagnosis and Decision Making: Overview and Implications | KFF
- https://arxiv.org/pdf/2204.10672 – Systematic_Review_with_figs
- https://www.mdpi.com/2073-4425/14/10/1840 – Population Pharmacogenomics for Health Equity
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10747429/ – The Intersection between Pharmacogenomics and Health Equity: A Case Example
- https://www.mdpi.com/1999-4923/15/7/1923 – Race, Ethnicity, and Pharmacogenomic Variation in the United States and the United Kingdom
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10289261/ – Editorial: The role of pharmacogenomics in addressing health disparities: the path, the promise, and the barriers
- https://scholarworks.umt.edu/cgi/viewcontent.cgi?article=13088&context=etd – EQUITABLE PHARMACOGENETIC TESTING IMPLEMENTATION FOR RURAL AND UNDERSERVED POPULATIONS
- https://www.mdpi.com/2075-4426/12/12/2046 – Patients’ Perspectives of Factors That Influence Pharmacogenetic Testing Uptake: Enhancing Patient Counseling and Results Dissemination
- https://www.nature.com/articles/s41525-021-00253-1 – Underrepresented patient views and perceptions of personalized medication treatment through pharmacogenomics – npj Genomic Medicine
- https://www.nature.com/articles/s41467-024-45032-5 – Implementing community-engaged pharmacogenomics in Indigenous communities – Nature Communications
- https://cpt.uchicago.edu/diversity-project/ – Diversity Project | Center for Personalized Therapeutics