Pharmacogenetic testing has emerged as one of the most exciting frontiers in personalized medicine. By analyzing a patient’s genetic makeup, these tests promise to guide treatment decisions, improve drug safety, and reduce costly trial-and-error prescribing. The rapid growth of PGx testing is fueled by increasing scientific discoveries, commercial test offerings, and the demand for precision healthcare. For healthcare providers, payers, and patients alike, the potential of pharmacogenomic tests feels transformative.
But alongside this growth comes scrutiny. The U.S. Food and Drug Administration (FDA) has repeatedly cautioned laboratories and companies against making unverified or misleading claims about the clinical impact of their tests. In warning letters and public statements, the FDA has made it clear: suggesting that a genetic test can predict how a patient will respond to a drug—without sufficient evidence or FDA review—is a regulatory red flag. These actions underscore the importance of accuracy and compliance in a rapidly evolving market.
For executives and marketers in this space, the message is simple but critical: tread carefully. While innovation drives opportunity, overstepping with unsupported claims can invite enforcement, damage credibility, and stall growth. Navigating FDA guidance is therefore not just a legal necessity, but a business imperative.
The FDA’s Position on Pharmacogenomic Claims
The FDA plays a central role in overseeing the safety and accuracy of genetic and pharmacogenetic testing. Any test marketed with claims that influence clinical decision-making typically falls under the agency’s authority, particularly if it is intended to guide treatment or predict patient response. This oversight ensures that only tests with sufficient scientific evidence and proper FDA review can be promoted as clinically actionable.
Enforcement actions have shown how seriously the FDA takes this responsibility. A well-known case involved Inova MediMap, a series of pharmacogenomic tests marketed with claims about drug response prediction. The FDA determined that these claims lacked adequate validation, resulting in a warning letter requiring the company to halt unapproved marketing.
Such actions highlight why “predictive” or “treatment-guiding” statements trigger scrutiny. Without peer-reviewed evidence and regulatory clearance, claims can mislead clinicians and patients, raising both safety and compliance risks for test developers.
The Science Behind Pharmacogenomics
Pharmacogenetic testing explores how genetic variation influences drug response. Enzymes in the cytochrome P450 (CYP450) family, such as CYP2C19 and CYP2D6, are central to drug metabolism. Variants in these genes determine whether a person is a poor, normal, or ultra-rapid metabolizer, directly affecting drug efficacy and risk of side effects. Other clinically important genes include TPMT and DPD, which influence tolerance to thiopurines and fluoropyrimidines, and HLA variants like HLA-B*57:01, linked to severe hypersensitivity reactions.
The promise of PGx testing is clear: safer prescribing, fewer adverse drug events, and more effective treatment. Yet limitations remain. While some gene–drug pairs are well validated, others lack sufficient evidence across diverse populations. This explains why FDA guidance urges caution—unproven claims risk misleading clinicians and patients. For companies, rigorous evidence and peer-reviewed validation are essential not only for regulatory acceptance but also for building credibility in precision medicine.
Regulatory Landscape and Enforcement Trends
The FDA plays a central role in ensuring that pharmacogenetic testing (PGx testing) is both safe and reliable. While the science behind pharmacogenomic tests advances rapidly, regulation lags, creating a delicate balance between innovation and oversight. Companies must understand where the FDA draws its boundaries—particularly around marketing claims—to avoid enforcement actions.
FDA Authority Over Genetic Tests
- Laboratory-Developed Tests (LDTs): Traditionally under “enforcement discretion,” but the FDA intervenes when LDTs are promoted with treatment-guiding claims.
- Companion Diagnostics: The gold standard, fully reviewed by the FDA and directly tied to a drug label. These tests have clear pathways for clinical use.
- Unapproved PGx Panels: Frequently fall into a gray zone; claims about drug efficacy or safety without FDA review often trigger regulatory attention.
Key Milestones and Enforcement Signals
| Area | Impact on PGx Testing |
| FDA guidance on genetic tests | Sets expectations for analytical validity and evidence of utility |
| Approval of companion diagnostics | Provides a model for validated pharmacogenomic claims |
| Inova MediMap warning letter | Clear example of FDA action against unsupported predictive claims |
| Ongoing LDT regulation debate | Continues to create uncertainty for test developers |
Preemptive vs. Reactive Testing: A Regulatory Lens
The distinction between preemptive and reactive testing illustrates why the FDA is cautious about marketing claims.
- Preemptive testing genotypes patients before they need medication, storing data for future prescribing decisions. While attractive for its efficiency, this model often lacks immediate clinical context. Without strong evidence showing routine benefit across populations, the FDA views broad marketing of preemptive PGx panels as premature.
- Reactive testing, by contrast, is ordered when a prescribing decision is imminent. Because the test is tied directly to a clinical action—such as choosing the right dose of clopidogrel—this approach better aligns with current FDA expectations for demonstrated utility.
| In short, regulatory scrutiny isn’t just about the gene or the technology—it’s about the context of use. The FDA is more likely to challenge preemptive claims that overstate clinical value, while reactive testing remains the safer path until more evidence supports broader adoption. |
Application of Pharmacogenomics: Genes and Drugs
The FDA has steadily expanded the number of drugs with pharmacogenomic (PGx) labeling, covering critical therapeutic areas like cardiology, oncology, psychiatry, and infectious disease. Understanding which genes matter—and how their variants affect drug response—helps executives, clinicians, and laboratories appreciate why scientific rigor and regulatory alignment are non-negotiable.
The FDA’s Table of Pharmacogenomic Biomarkers in Drug Labeling now includes more than 200 drugs, spanning enzymes like CYP450 isoforms, TPMT, DPYD, and UGT1A1. Below, we zoom into four of the most clinically significant and frequently cited examples: CYP2C19 with clopidogrel, CYP2D6 with codeine/tamoxifen, TPMT with thiopurines, and DPYD with fluoropyrimidines.
CYP2C19 and Clopidogrel
Clopidogrel (Plavix), an antiplatelet agent, must be metabolized by CYP2C19 to its active form. Patients who are poor metabolizers (PMs) produce less active drug, leaving them at risk for stent thrombosis and other cardiovascular events.
- FDA Note: A Black Box warning explicitly highlights reduced efficacy in CYP2C19 PMs. Alternative therapies such as prasugrel or ticagrelor are recommended for these patients.
- Clinical Relevance: Genetic testing before prescribing can prevent potentially life-threatening outcomes.
CYP2D6 & Multi-Drug Implications
CYP2D6 affects the metabolism of over 70 FDA-recognized drugs. This diversity makes a once-per-lifetime PGx test highly impactful.
Why CYP2D6 matters:
- Codeine & Tramadol: Poor metabolizers = no pain relief; ultra-rapid metabolizers = morphine toxicity risk.
- Tamoxifen: Requires CYP2D6 activation to endoxifen; poor metabolizers risk reduced anticancer efficacy.
- Psychiatric medications: Variability in SSRI, TCA, and antipsychotic metabolism directly impacts dosing, side effects, and adherence.
- Beta-blockers & antiarrhythmics: CYP2D6 phenotype influences therapeutic response.
| FDA Note: Tetrabenazine (another CYP2D6 substrate) carries a mandatory genotyping recommendation above certain doses. This signals the FDA’s expectation that testing is integrated into clinical workflows when safety risks are high. |
Breadth of CYP2D6 Substrates
| Therapeutic Area | Examples | Clinical Relevance |
| Psychiatric drugs | SSRIs (paroxetine, fluoxetine, escitalopram), TCAs, antipsychotics (risperidone, aripiprazole) | Altered efficacy, risk of side effects |
| Cardiovascular | Beta-blockers (metoprolol, propranolol, carvedilol), antiarrhythmics (propafenone) | Dose-response variability |
| Analgesics | Codeine, tramadol | Risk of toxicity or non-response |
| Oncology | Tamoxifen, gefitinib | Impact on treatment outcomes |
TPMT and Thiopurine Drugs
Thiopurine drugs (azathioprine, 6-mercaptopurine, thioguanine) are used in leukemia, inflammatory bowel disease, and transplant medicine.
- Risk: Patients with low or absent TPMT activity cannot inactivate thiopurines effectively, leading to severe, potentially fatal myelosuppression.
- FDA Note: Package inserts recommend TPMT (and NUDT15) testing before initiating therapy, especially at standard or high doses.
- Clinical Use: Dosing adjustments—sometimes reductions of 90%—are guided by TPMT/NUDT15 status.
DPYD and Fluoropyrimidines
Fluoropyrimidines (5-fluorouracil, capecitabine) remain cornerstones of oncology. Their metabolism depends on DPD (encoded by DPYD).
- Risk: Deficiency in DPD leads to severe, dose-limiting toxicity including mucositis, neutropenia, and neurotoxicity.
- FDA Note: Labeling for capecitabine and fluorouracil references this risk, though explicit pre-testing is not always mandated.
- Clinical Momentum: European regulators increasingly recommend routine DPYD testing prior to therapy, and the FDA is closely monitoring evidence.
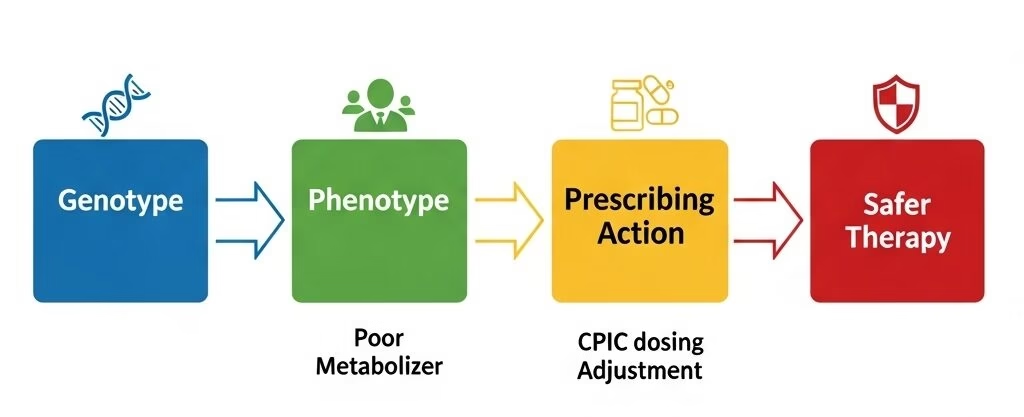
Guidelines & Implementation: The Role of CPIC
The Clinical Pharmacogenetics Implementation Consortium (CPIC) is an international organization that creates and publishes evidence-based guidelines to help clinicians understand and use pharmacogenetic test results to optimize drug therapy. Its primary goal is to empower healthcare providers to use genetic information to make more informed decisions about drug selection and dosing, thereby improving patient safety and treatment efficacy. By translating complex genetic data into actionable clinical recommendations, CPIC facilitates the practical application of personalized medicine in routine medical practice.
What CPIC Does
- Focuses on how to use genetic results, not whether to test.
- Provides evidence-based dosing recommendations based on genotype/phenotype.
- Guidelines endorsed by AMP, ASCPT, ASHP, and other professional societies.
Metabolizer Status
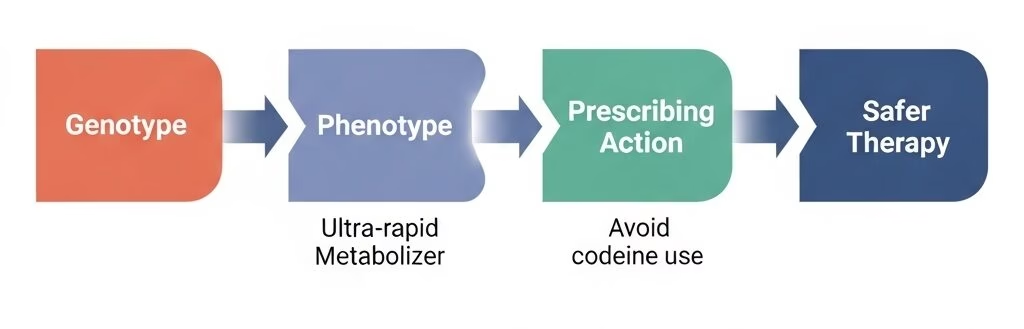
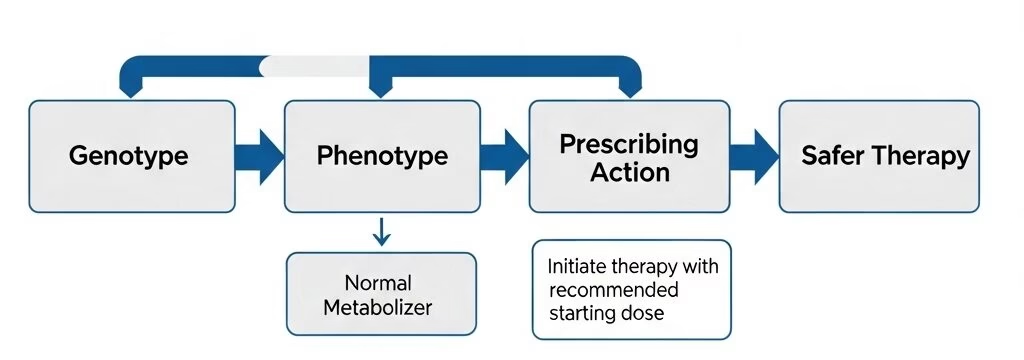
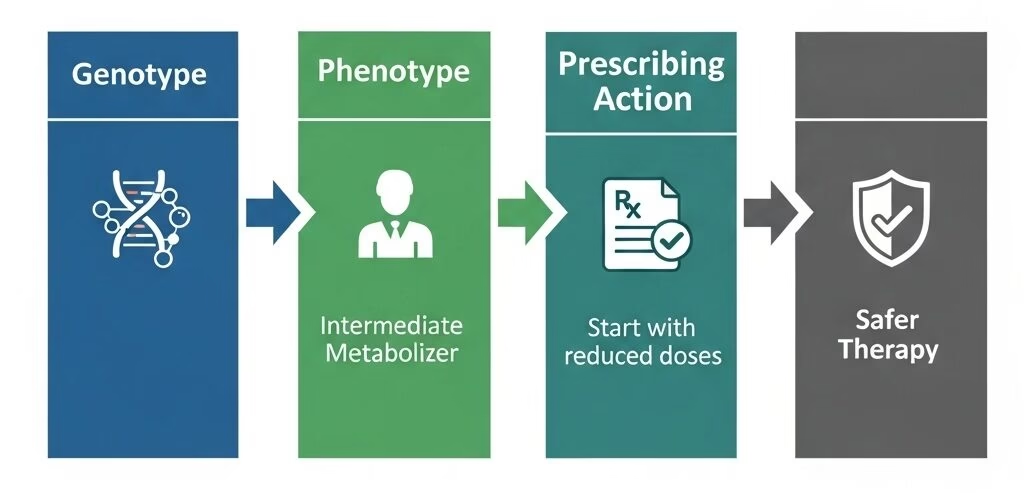
Based on their genetic makeup, individuals are classified into different metabolizer phenotypes, which affects how quickly or slowly they process certain drugs. These phenotypes include:
- Ultra-rapid Metabolizer (URM): Metabolize drugs much faster than normal.
- Normal Metabolizer (NM): Have typical drug metabolism.
- Intermediate Metabolizer (IM): Metabolize drugs more slowly than normal.
- Poor Metabolizer (PM): Metabolize drugs very slowly or not at all.
Level of Recommendation
CPIC guidelines provide a strength of recommendation for each action. This helps clinicians understand how strong the evidence is for a particular therapeutic adjustment. The levels are typically categorized as:
- Strong: A high degree of certainty that the recommended action will result in a net benefit for the patient.
- Moderate: A reasonable level of confidence that the recommended action will be beneficial, but the evidence isn’t as robust as for a “strong” recommendation.
- Optional: Recommendations with limited evidence or with potential for controversy, suggesting that the clinical decision should be made on a case-by-case basis.
CPIC Recommendation Strength
| Strength | Meaning | Example |
| Strong | Genetic result should always inform prescribing | Avoid codeine in CYP2D6 ultra-rapid metabolizers |
| Moderate | Genetic result can guide prescribing, but alternatives exist | Dose adjustment for TCAs in CYP2D6 IMs/PMs |
| Optional | Genetic info may be used, but evidence is weaker | Adjust celecoxib dose in CYP2C9 PMs |
Key Gene–Drug Pairs Covered by CPIC
| Gene | Drug(s) | PGx Impact | CPIC Guidance |
| CYP2C19 | Clopidogrel | Poor metabolizers form less active metabolite → ↓ efficacy | Use alternative P2Y12 inhibitor |
| CYP2D6 | Codeine | Ultra-rapid metabolizers risk overdose; PMs get no effect | Avoid codeine, select alternative analgesic |
| CYP2C9 + VKORC1 | Warfarin | Variants influence bleeding risk and dosing | Adjust initial dose per genotype |
| TPMT/NUDT15 | Thiopurines (azathioprine, 6-MP) | Reduced enzyme activity → toxicity | Start at reduced dose or use alternative |
| DPYD | 5-FU, Capecitabine | Reduced enzyme activity → life-threatening toxicity | Avoid or reduce dose in poor metabolizers |
| HLA-B*15:02 | Phenytoin, Carbamazepine | Severe skin reactions (SJS/TEN) | Avoid in carriers |
Quick List: CPIC’s Most Common Clinical Applications
✅ Antiplatelets (clopidogrel)
✅ Antidepressants (SSRIs, TCAs)
✅ Analgesics (codeine, tramadol)
✅ Anticoagulants (warfarin)
✅ Antiepileptics (phenytoin, carbamazepine)
✅ Oncology drugs (thiopurines, fluoropyrimidines)
Across the globe, professional bodies have reached differing but complementary conclusions on the role of pharmacogenetic testing in care. The Dutch Pharmacogenetics Working Group (DPWG) has taken one of the strongest positions, recommending clinical implementation of just four well-validated DPYD variants in fluoropyrimidine therapy. In the U.S., the FDA has gone further by publishing association tables for numerous genes, though it emphasizes that not all evidence is ready for clinical decision-making—TYMS testing, for instance, remains unsupported.
Cardiology guidelines from the American College of Cardiology Foundation and the American Heart Association reflect a cautious stance: while CYP2C19 polymorphisms clearly influence clopidogrel metabolism, routine genetic testing is not recommended outside of high-risk scenarios, leaving clinicians to rely on judgment and individual risk profiles. The American Academy of Neurology echoes this caution in pain management, noting that more original research is needed before opioids can be tailored through PGx testing. Similarly, the AACC Academy suggests testing should not be routine but can be useful in cases of repeated treatment failure or unexplained adverse drug reactions.
| Note: These guidelines highlight a consistent theme: pharmacogenetic testing is powerful where evidence is robust but premature when applied too broadly. The most sustainable strategy is to emphasize validated use cases while acknowledging the limits of current science. |
How Clinicians Use Genotype to Guide Drug Dosing
Clinicians use a patient’s genotype to predict their metabolizer phenotype, which in turn guides drug dosing and prescribing decisions. By identifying genetic variations in key enzymes like the Cytochrome P450 (CYP450) family, clinicians can determine if a patient is an ultra-rapid, normal, intermediate, or poor metabolizer of a specific drug. For example, if a patient is a CYP2D6 poor metabolizer, they break down drugs like metoprolol very slowly. This can lead to the drug building up to toxic levels, potentially causing a dangerous drop in blood pressure and heart rate. In this case, a clinician would likely prescribe a lower-than-normal starting dose of metoprolol or choose an alternative medication. This personalized approach reduces the risk of adverse drug reactions, avoids trial-and-error prescribing, and ensures the patient receives an effective and safe dose from the outset.
Identifying Patients for Pharmacogenomics Testing
Identifying candidates for pharmacogenetic (PGx) testing involves a multifaceted approach, considering both patient-specific factors and broader health system considerations.
- Patient Requests: Individual patients may seek testing due to a history of adverse drug reactions, a desire to avoid “trial-and-error” prescribing, or an interest in personalized care.
- Prevalence and Clinical Impact: Health systems consider the prevalence of a medication’s use and the likelihood of an actionable result—a result that would change prescribing. This includes assessing the frequency of specific genetic variants in the patient population. For example, the odds ratio for severe skin reactions from carbamazepine is over 1000 in individuals with the HLA-B*15:02 allele.
- Severity of Adverse Outcomes: The potential severity of an adverse event is a key factor. For instance, clopidogrel non-response in CYP2C19 poor metabolizers can lead to serious and potentially fatal cardiovascular events, making genetic testing for this drug a higher priority than for a drug with less severe potential side effects.
- Alternative Treatments: Clinicians evaluate the availability and risks of alternative treatments. PGx testing is most valuable when the results can directly lead to a change in care, such as switching to a safer or more effective drug. If alternative treatments are not accessible or pose their own unacceptable risks, the value of the test may be limited.
- Cost and Coverage: The cost of testing and insurance coverage heavily influence adoption. While cash prices for multigene panels often range from $300 to $500, coverage can be variable. In the U.S., Medicare has recently updated local coverage determinations to cover PGx testing for over 100 medications, indicating a growing trend towards broader coverage.
Pharmacogenomics Coverage Policy & What Is (Not) Medically Necessary
The medical necessity of pharmacogenomic (PGx) testing depends on its application to an individual’s specific medication therapy. For most genes, testing is considered medically necessary only once per lifetime to guide therapy selection or dosing for a list of approved medications. However, testing is not considered medically necessary for a patient who has received a liver transplant.
What testing is considered “medically necessary”
A test is considered medically necessary to aid in therapy selection and/or dosing for a wide range of medications, each linked to a specific set of genes. The following are examples of such tests:
- CYP2D6 Genotype: Tested for drugs like codeine, tramadol, and various antidepressants such as venlafaxine and paroxetine.
- CYP2C19 Genotype: Tested for medications including clopidogrel, citalopram, and proton pump inhibitors (PPIs) like omeprazole (if the patient has an active H. pylori infection).
- CYP2D6 & CYP2C19 Genotypes: Both genes are tested together for specific tricyclic antidepressants like amitriptyline and clomipramine.
- CYP2C9 Genotype: Tested for drugs such as celecoxib, warfarin, and meloxicam.
- TPMT & NUDT15 Genotypes: Tested for thiopurine drugs like azathioprine and mercaptopurine.
- DPYD Genotype: Tested for chemotherapy agents such as fluorouracil and capecitabine.
- Human Leukocyte Antigen (HLA): Specific HLA genotypes are tested before prescribing drugs like abacavir (HLA-B*57:01) and allopurinol (HLA-B*58:01).
- Other Genes: Testing for genes like CYP3A5 (for tacrolimus), UGT1A1 (for irinotecan), and BCHE (for mivacurium or succinylcholine) is also deemed medically necessary for their respective drug therapies.
What is excluded (not medically necessary)
The following types of pharmacogenetic testing are not considered medically necessary:
- Repeated Testing: Genotyping the same gene more than once per lifetime, even for a different medication, is not covered. An exception is made for HLA variants, where a specific variant is tested for a specific medication.
- General Population Screening: Testing the general population without a specific medication indication is not covered.
- Inpatient Testing: PGx testing in a patient who has received a liver transplant is not covered.
- Testing for Statin Myopathy: Genetic testing for variants in the SLCO1B1 gene to identify a risk of statin-induced myopathy is not considered medically necessary.
- Multi-Gene Panels: Panel testing for situations not explicitly addressed in the medically necessary list is not covered due to a lack of confirming scientific literature.
- Proton Pump Inhibitors (PPIs): Testing for PPI therapies is only covered if the patient has an active H. pylori infection.
Marketing Risks and Common Pitfalls
As the field of pharmacogenomics (PGx) grows, so does the regulatory scrutiny from the FDA. For companies, navigating this landscape requires a deep understanding of what constitutes acceptable marketing claims versus dangerous overreach.
Examples of Overreach in PGx Marketing
Overreach in PGx marketing occurs when companies make unverified or misleading claims that lack sufficient scientific evidence or regulatory review. These claims often suggest that a genetic test can definitively predict a patient’s response to a drug or guide treatment decisions without proper validation. The FDA views these “predictive” or “treatment-guiding” statements as a significant regulatory red flag. Without peer-reviewed evidence and regulatory clearance, such claims can mislead both clinicians and patients, posing safety risks and inviting enforcement action.
| Case Study: Inova MediMapA well-known example of regulatory enforcement is the case involving Inova MediMap. This company marketed a series of pharmacogenomic tests with claims that they could predict drug response. The FDA investigated and determined that these claims lacked adequate validation. As a result, the FDA issued a warning letter requiring the company to immediately halt its unapproved marketing of the tests. This case serves as a clear illustration of the FDA’s stance against unsupported predictive claims. |
Lessons Learned from Enforcement Actions
Enforcement actions like the Inova MediMap case teach critical lessons for companies in the PGx space. The primary takeaway is that treading carefully is not just a legal necessity, but a business imperative.
- Evidence is everything: Marketing claims must be backed by rigorous evidence and peer-reviewed validation. Without this, companies risk damaging their credibility and inviting regulatory action.
- Predictive vs. Contextual Claims: The FDA is particularly cautious about preemptive testing, which tests patients before they need a specific drug. The agency considers marketing for such broad panels to be premature without strong evidence of a clear clinical benefit. In contrast, reactive testing—ordered for an imminent prescribing decision—is more aligned with the FDA’s expectations for demonstrated clinical utility.
- Compliance is a business imperative: Overstepping regulatory boundaries with unsupported claims can lead to enforcement actions that can stall growth and damage a company’s reputation in the rapidly evolving precision medicine market.
Leveraging FDA-Compliant Marketing Strategies For Pharmacogenomic Tests
A core principle of successful PGx marketing is to align all strategies with FDA guidance. This involves a shift from making bold, unverified claims to focusing on educational content and evidence-based information.
- Avoid Predictive Claims Without Evidence: Never market a PGx test with claims that it can definitively predict a patient’s response to a drug without robust, peer-reviewed scientific evidence and, where applicable, regulatory clearance.
- Emphasize Research or Informational Use: For tests where evidence is still emerging, frame their purpose as a tool for research or for providing clinicians with additional informational context, rather than as a definitive guide for prescribing.
- Collaborate with Regulatory Counsel: Proactively work with legal and regulatory experts to ensure all marketing materials and claims are compliant. This can help identify potential red flags before they lead to enforcement actions.
- Keep Up-to-Date with FDA Guidance: The regulatory landscape is constantly evolving. Regularly monitor FDA websites and publications for new guidance, warning letters, and approved companion diagnostics to understand current expectations.
- Implement Internal Compliance Training: Educate marketing, sales, and clinical teams on the importance of regulatory compliance and the specific language to avoid. This creates a culture of accountability and reduces the risk of making unsupported claims.
- Document Scientific Evidence: Maintain a well-organized repository of all scientific literature, clinical studies, and data that support the claims made about a test. This documentation is crucial for responding to any regulatory inquiries.
- Seeking FDA Review: For tests intended to be used as a companion diagnostic, actively pursue FDA review and approval. This provides the highest level of validation and allows for robust, on-label marketing claims that can be directly tied to a drug’s use.
Conclusion
Pharmacogenomics holds immense promise for transforming medicine by moving from a one-size-fits-all approach to a personalized model of care. The work of organizations like CPIC provides a crucial roadmap for clinicians, translating complex genetic data into actionable prescribing decisions that improve patient safety and treatment efficacy. However, as the field grows, it is imperative to address the challenges of inconsistent coverage and, most importantly, the risks of unsupported marketing claims. By upholding the highest standards of scientific integrity, focusing on evidence-based strategies, and adhering to regulatory guidance, the industry can build trust with patients and providers alike, ensuring that the transformative potential of personalized medicine is realized safely and responsibly.
References
- https://www.researchgate.net/figure/FDA-approved-drugs-with-pharmacogenomic-information-in-the-labeling_tbl1_254276834
- https://www.southcarolinablues.com/web/public/brands/medicalpolicy/external-policies/pharmacogenetic-testing/
- https://www.uptodate.com/contents/overview-of-pharmacogenomics
- https://www.uptodate.com/contents/human-leukocyte-antigens-hla-a-roadmap
- https://www.fda.gov/news-events/press-announcements/fda-converts-novel-alzheimers-disease-treatment-traditional-approval
- https://www.fda.gov/news-events/press-announcements/fda-converts-novel-alzheimers-disease-treatment-traditional-approval
- https://www.uptodate.com/contents/clopidogrel-resistance-and-clopidogrel-treatment-failure
- https://s3.amazonaws.com/myriad-web/Managed+Care/CPGx-approach.pdf
- https://s3.amazonaws.com/myriad-web/Managed+Care/GeneSight-ExecutiveSummary.pdf
- https://investor.myriad.com/news-releases/news-release-detail/24211/
- https://www.mayocliniclabs.com/test-catalog/Overview/610057
- https://sema4.com/products/test-catalog/comprehensive-pharmacogenetic-genotyping-panel/#
- https://www.accessdata.fda.gov/cdrh_docs/reviews/K043576.pdf
- https://oneome.com/rightmed-test/#genes-covered
- https://www.ncbi.nlm.nih.gov/gtr/tests/552110.3/performance-characteristics/





