Healthcare is changing, and genetics is helping lead the way. Pharmacogenomics, or PGx, looks at how a person’s genes affect the way they respond to medications, helping doctors pick the right drug and dose for each individual.
For Veterans, who often juggle chronic conditions, mental health challenges, pain management, and multiple medications, PGx can make a real difference. By considering each Veteran’s unique genetic makeup, treatments can be more effective, side effects can be reduced, and everyday life can feel a little easier.
The PHASER Initiative
The PHASER (Pharmacogenomic Testing for Veterans) program is the VA’s major effort to bring clinical PGx testing to Veterans at scale. Launched in 2019, PHASER applies a panel of gene tests to Veterans so that their medical records hold actionable genetic information related to drug response. Unlike research studies, PHASER is a clinical program: test results are meant to guide everyday prescribing decisions.
PHASER provides an end-to-end implementation, from ordering the test to returning results in the electronic health record, supporting provider education, and offering decision-support systems. Early results are promising, and the VA is expanding the gene panels and improving turnaround times. Many Veterans are prescribed medications where gene-drug interactions are relevant, so having genetic information readily available allows clinicians to make informed decisions and avoid trial-and-error prescribing.
PGx for Veterans Can’t be Overlooked
For Veterans managing conditions such as depression, chronic pain, or heart disease, pharmacogenomics has been a real breakthrough. By looking at a Veteran’s genetic makeup, clinicians can better match medications to each individual, helping reduce side effects, improve effectiveness, and enhance overall quality of life. Surgical teams are also beginning to use PGx to identify risks before procedures, making the operating room safer and reducing the chances of complications.
Chronic Conditions & Multiple Medications
- Veterans often deal with complex health issues like chronic pain, cardiovascular disease, PTSD, and depression.
- Many are on long-term medications, and it’s common to take several at once (polypharmacy).
- Taking multiple drugs increases the risk of interactions, side effects, and treatment failures.
- Genetic differences can further affect how medications are metabolized or tolerated. PGx helps reduce these risks by guiding the choice of drug and dose based on each Veteran’s biology.
PTSD, Mental Health, and Pain Management
Medications for mental health conditions, including antidepressants, antipsychotics, and mood stabilizers, often vary in effectiveness from person to person, and side effects can be serious. PGx helps shorten the trial-and-error process, allowing clinicians to find the most effective medication faster and with fewer unwanted effects. Pain management, whether for chronic conditions or around surgical procedures, is another area where PGx is proving valuable, helping to minimize complications and improve outcomes.
The Risk Profile
- Treatments that aren’t well-matched to the patient can prolong symptoms and reduce quality of life.
- Adverse reactions may lead to hospitalization or other serious complications.
- Ineffective medications increase healthcare costs through wasted prescriptions, follow-ups, and managing preventable complications.
- For Veterans with service-related injuries or multiple health conditions, the stakes are even higher, making the precision of PGx especially important.
Implementation of PGx in Veteran Care
Since its pilot launch, PHASER has steadily expanded across the VA. The program now includes larger gene panels and faster turnaround times, ensuring test results are ready when clinicians need them. Integration into the electronic health record allows prescribing systems to reference PGx data directly, while point-of-care decision-support alerts help clinicians act on the results effectively.
Provider education is a key part of the program, equipping physicians, pharmacists, and other clinicians with the knowledge to interpret and apply PGx results. The VA has also built quality improvement efforts into the initiative, identifying and addressing barriers such as workflow challenges, training gaps, and IT integration.
Early outcomes indicate that PGx testing is already helping Veterans switch to medications better suited to their biology, reducing side effects and improving quality of life. The VA plans to continue expanding PGx adoption nationwide, with longer-term integration of AI tools and broader training initiatives.
Looking Ahead
For Veterans, PGx represents a powerful tool to optimize medication safety and effectiveness, particularly for those managing multiple medications or complex conditions. Health systems can learn from the VA’s implementation model, which demonstrates the importance of integrating genetic data into clinical workflows, providing decision support, and educating clinicians.
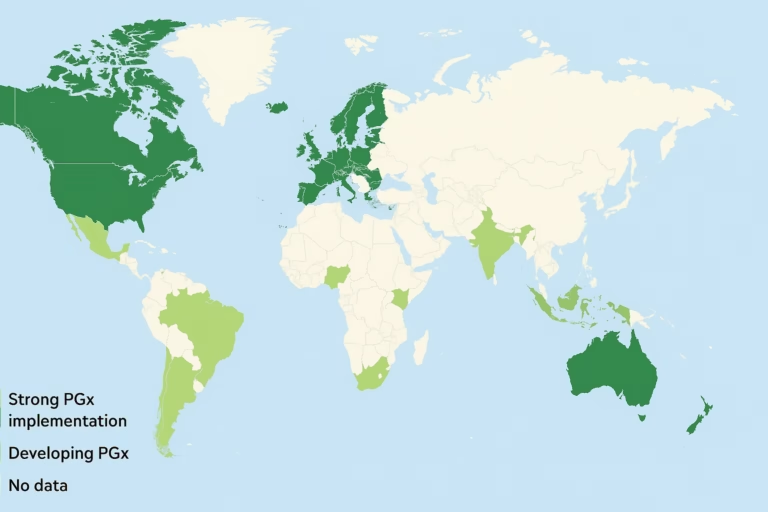
The PHASER initiative may serve as one of the largest real-world examples of PGx implementation, offering lessons for other health systems worldwide. As gene panels expand and turnaround times shorten, the practical value of pharmacogenomics will grow. Success in this case will depend on systems that connect genetic data to actionable prescribing decisions, ensuring that Veterans receive the right drug, at the right dose, at the right time.
References
- https://news.va.gov/142488/va-expands-precision-medicine-pharmacogenomics/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12360799/
- https://www.va.gov/phoenix-health-care/programs/phaser/