Nearly half of the claims submitted for pharmacogenomic testing are reimbursed, with a significant disparity in reimbursement rates based on the type of test and payer policies.
Pharmacogenomic (PGx) testing has revolutionized precision medicine by enabling healthcare providers to tailor medication choices and dosages based on a patient’s genetic profile. Despite its clinical benefits, reimbursement remains a challenge.
The overall reimbursement rate for PGx tests was found to be 46%, with testing panels reimbursed at a significantly higher rate than single gene tests. Understanding these patterns is crucial for optimizing billing practices and improving access to PGx testing, ultimately enhancing health outcomes.
The Current Landscape of Pharmacogenomic Testing
Pharmacogenomic testing is revolutionizing healthcare by tailoring medication plans to individual genetic profiles. This approach has shown significant promise in improving patient outcomes by reducing adverse reactions and enhancing the efficacy of treatments.
What is Pharmacogenomic Testing?
Pharmacogenomic testing, also known as PGx testing, involves analyzing a patient’s genetic data to predict their response to certain medications. This is achieved by examining variations in genes that code for drug-metabolizing enzymes, drug transporters, and drug targets. By understanding how an individual’s genetic profile affects their response to medication, healthcare providers can make more informed decisions about treatment plans.
The clinical applications of pharmacogenetic testing are vast, spanning multiple specialties including cardiology, psychiatry, pain management, oncology, and infectious disease. As a key component of precision medicine, PGx testing represents a shift away from the traditional “one-size-fits-all” approach to medication prescribing, toward individualized therapy based on genetic profiles.
The benefits of pharmacogenomic testing include improved medication safety and effectiveness, as well as reduced hospital admissions and emergency department visits. As the field continues to evolve, it is likely that PGx testing will become an increasingly important tool in healthcare, enabling providers to deliver more personalized and effective care.
Some key aspects of pharmacogenomic testing include:
- Analyzing specific genes that influence how individuals metabolize and respond to medications.
- Examining genetic variations that impact medication efficacy and safety.
- The evolution from single-gene assays to comprehensive multi-gene panels.
- Applications across multiple drug classes and therapeutic areas.
The Current Landscape of Pharmacogenomic Testing
The integration of pharmacogenomic testing into healthcare is transforming patient care by providing personalized treatment options based on genetic information. This approach has gained significant attention in recent years due to its potential to improve health outcomes and reduce healthcare costs.
Clinical Applications and Benefits
Pharmacogenomic testing, also known as PGx testing, has numerous clinical applications. It provides actionable information for various medication classes, enabling healthcare providers to make informed prescribing decisions. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published guidelines covering high-evidence gene-drug pairs, which support the use of PGx testing in clinical practice.
- PGx tests offer insights into genetic variations affecting drug metabolism, helping clinicians adjust dosages or choose alternative medications.
- Key applications include CYP2C19 testing for antiplatelet therapy, CYP2D6 testing for opioid prescribing, and combined CYP2C19/CYP2D6 testing for antidepressant selection.
- The implementation of pharmacogenetic tests has demonstrated improved health outcomes, including reduced adverse drug reactions and enhanced medication efficacy.
The benefits of PGx testing are evident across multiple specialties. However, reimbursement challenges continue to limit its widespread adoption.
| Gene-Drug Pair | Clinical Application | Benefit |
|---|---|---|
| CYP2C19-clopidogrel | Antiplatelet therapy | Reduced risk of cardiovascular events |
| CYP2D6-opioids | Opioid prescribing | Improved pain management, reduced risk of overdose |
| CYP2C19/CYP2D6-SSRIs | Antidepressant selection | Enhanced efficacy, reduced risk of adverse reactions |
As the evidence supporting PGx testing continues to grow, its adoption is expected to increase, leading to better patient outcomes and more efficient healthcare delivery.
The Current Landscape of Pharmacogenomic Testing
Clinical practice is witnessing a significant shift with the adoption of pharmacogenomic (PGx) testing. As genetic testing technology advances, PGx testing is becoming more accessible and integrated into healthcare delivery.
The growth of PGx testing in clinical practice has been substantial over the past decade. Initially confined to academic medical centers, PGx testing has expanded to community hospitals and outpatient settings, increasing its reach and impact on patient care.
Growth of PGx Testing in Clinical Practice
Several factors have contributed to this growth. Technological advancements have reduced the cost of testing while increasing the breadth of genetic variants that can be assessed. This has made comprehensive panels more accessible, enabling healthcare providers to tailor treatment plans to individual patients based on their genetic profiles.
- The adoption of PGx testing has grown significantly, with implementation expanding beyond academic medical centers.
- Technological advancements have reduced testing costs and increased the scope of genetic variants assessed.
- Despite clinical evidence supporting PGx testing, financial barriers remain a significant obstacle to widespread implementation.
- Patients are more likely to undergo testing when insurance coverage is available, highlighting the importance of reimbursement.
The gap between clinical utility and reimbursement policies has created a challenging environment for providers and laboratories seeking to incorporate PGx testing into routine care. Ensuring that PGx testing is reimbursed by insurance providers is crucial for its continued adoption and for making personalized medicine more accessible to patients.
Understanding Reimbursement for Pharmacogenomic Testing
Understanding the reimbursement landscape for pharmacogenomic testing is crucial for providers and laboratories. The process involves multiple stakeholders who play significant roles in determining coverage and reimbursement policies.
Key Stakeholders in the Reimbursement Process
The reimbursement landscape for pharmacogenomic testing involves several key stakeholders, including commercial insurance companies, Medicare, Medicaid, laboratory benefit managers (LBMs), and healthcare providers. Each of these stakeholders has a distinct role in shaping reimbursement policies.
- Commercial Payers: Develop their own medical policies for coverage determination, often based on clinical evidence and guidelines.
- Medicare: Coverage is typically determined through Local Coverage Determinations (LCDs) by Medicare Administrative Contractors.
- Laboratory Benefit Managers (LBMs): Increasingly influence coverage decisions by evaluating the clinical validity and utility of tests.
- Patient Advocacy Groups and Professional Medical Societies: Play crucial roles in shaping reimbursement policies through guideline development and advocacy efforts.
Health plan medical policies that align with clinical practice guidelines, FDA recommendations, and published evidence are critical in enabling patient access to pharmacogenomic testing. However, inconsistent insurance coverage remains a challenge despite evidence suggesting that testing is cost-effective for many drug-gene examples.
Understanding the perspectives and requirements of these stakeholders is essential for providers and laboratories seeking to navigate the reimbursement process successfully. By recognizing the roles of these key stakeholders, healthcare providers can better position themselves to secure reimbursement for pharmacogenomic testing.
Understanding Reimbursement for Pharmacogenomic Testing
Navigating the complexities of reimbursement for pharmacogenomic testing requires a deep understanding of billing codes and terminology. Pharmacogenomic testing, which involves analyzing genes to predict an individual’s response to certain medications, has become increasingly important in personalized medicine.
The process of reimbursement for these tests is multifaceted, involving various stakeholders and requiring precise coding for successful claims. Proper coding is critical for the reimbursement of pharmacogenomic testing, with Current Procedural Terminology (CPT) codes being the primary method for billing these services.
Billing Codes and Terminology
The use of accurate billing codes is essential for laboratories and healthcare providers to receive reimbursement for pharmacogenomic tests. Single-gene pharmacogenomic tests typically use specific CPT codes (e.g., 81225 for CYP2C19, 81226 for CYP2D6), while multi-gene panels may be billed using either individual gene codes or panel-specific Proprietary Laboratory Analyses (PLA) codes.
- Diagnosis codes (ICD-10-CM) significantly impact reimbursement success, with data showing that claims submitted with multiple relevant diagnosis codes have higher reimbursement rates.
- Understanding the relationship between CPT codes and diagnosis codes is essential, as certain combinations are more likely to result in successful reimbursement based on established medical necessity criteria.
- Laboratories and providers must stay current with coding updates, as new PLA codes are regularly added for specific pharmacogenomic panels, potentially affecting reimbursement strategies.
The specific genes offered and the CPT codes billed by laboratories, such as the UF Health Pathology lab, are outlined in detailed tables. For instance, Table 1 provides a breakdown of the genes and corresponding CPT codes used.
| Gene | CPT Code | Description |
|---|---|---|
| CYP2C19 | 81225 | CYP2C19 gene analysis |
| CYP2D6 | 81226 | CYP2D6 gene analysis |
| Multi-gene Panel | Various/PLA Code | Pharmacogenomic panel testing |
By understanding and accurately applying billing codes and terminology, healthcare providers and laboratories can improve their chances of successful reimbursement for pharmacogenomic testing.
Understanding Reimbursement for Pharmacogenomic Testing
The reimbursement landscape for pharmacogenomic testing is evolving, with significant variability across different payers and test types. Recent data from a comprehensive analysis of 1,039 outpatient claims reveals an overall reimbursement rate of 46% for PGx testing.
A closer examination of the data shows that PGx panels demonstrate substantially higher reimbursement rates (74%) compared to single-gene tests (43%). This suggests that comprehensive testing approaches may be more readily approved by payers.
Medicare Reimbursement Patterns
Reimbursement rates vary by payer type, with commercial insurance and Medicare both showing rates around 48%, while Medicaid averages 42% and other payers approximately 36%. The actual reimbursement amount typically ranges from 20-80% of the billed charge, with significant variations based on payer contracts and fee schedules.
| Payer Type | Reimbursement Rate |
|---|---|
| Commercial Insurance | 48% |
| Medicare | 48% |
| Medicaid | 42% |
| Other Payers | 36% |
Understanding these typical reimbursement rates can help laboratories and providers set appropriate expectations and develop financial models that account for expected payment patterns.
Key Takeaways:
- PGx panels are reimbursed at a significantly higher rate than single-gene tests.
- Reimbursement rates vary by payer type, with commercial insurance and Medicare showing higher rates.
- The actual reimbursement amount can range from 20-80% of the billed charge.
Insurance Coverage Landscape for PGx Tests
The evolution of Medicare’s coverage for PGx tests mirrors the growing importance of genetic testing in clinical practice. As PGx testing becomes more integral to personalized medicine, understanding Medicare’s coverage policies is crucial for healthcare providers and laboratories.
Since July 2020, Medicare Administrative Contractors (MACs) have been implementing more comprehensive coverage policies for PGx testing. The Molecular Diagnostic Services (MolDX) Program, administered by Palmetto GBA, has established a Local Coverage Determination (LCD) that covers numerous PGx tests when specific criteria are met. This development has significantly expanded Medicare coverage for PGx tests, increasing accessibility for over 48 million Medicare beneficiaries in the United States.
Medicare Coverage Policies
Medicare coverage policies generally rely heavily on Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines and FDA recommendations when determining medical necessity. Most MACs now provide coverage for both single-gene tests and multi-gene panels, though panels typically require additional documentation of medical necessity. Understanding the specific requirements of the MAC in your region is essential, as coverage policies can vary geographically despite the national Medicare program.
- Medicare coverage for PGx tests has expanded significantly since 2020.
- The MolDX Program has established an LCD covering numerous PGx tests.
- Coverage policies rely on CPIC guidelines and FDA recommendations.
- Most MACs cover single-gene tests and multi-gene panels with varying requirements.
For healthcare providers and laboratories, staying informed about these developments in reimbursement and coverage for PGx tests is crucial for navigating the complex landscape of genetic testing coverage.
Insurance Coverage Landscape for PGx Tests
The landscape of insurance coverage for pharmacogenomic (PGx) tests is complex and varies significantly across different payer types. This variability affects the reimbursement of PGx tests, making it challenging for healthcare providers and laboratories to navigate the system.
In the United States, the insurance coverage landscape for PGx tests is particularly diverse, with different payers having distinct policies regarding coverage and reimbursement rates. This diversity impacts patient access to PGx testing and the financial sustainability of these tests for healthcare providers.
Medicaid Coverage Variations
Medicaid coverage for PGx tests varies significantly across states, creating a complex patchwork of policies throughout the United States. State Medicaid programs have considerable autonomy in determining coverage policies, resulting in substantial geographic disparities in access to PGx testing.
- Some state Medicaid programs follow Medicare guidelines for coverage determination, while others have developed their own, often more restrictive criteria.
- Data shows that Medicaid plans generally have lower reimbursement rates for PGx tests compared to Medicare and commercial insurance.
- Providers serving Medicaid populations should be particularly attentive to state-specific coverage policies and prior authorization requirements to maximize reimbursement success.
Understanding these variations is crucial for healthcare providers and laboratories to ensure they are adequately prepared to navigate the complex landscape of PGx test reimbursement and provide accessible, high-quality care related to health issues.

Insurance Coverage Landscape for PGx Tests
Understanding commercial payer policies is crucial for navigating PGx test reimbursement. Commercial insurance coverage for PGx tests in the United States shows significant variability, with major national insurers having markedly different medical policies.
The landscape of private payer policies and PGx has been investigated over the last decade, with policies indicating coverage for single-gene testing approximately 45% of the time a specific gene test is mentioned in a medical policy. For instance, a study examined 41 policies and found that PGx tests were covered 18 out of 56 times testing was mentioned.
Commercial Payer Policies
Commercial payer policies for PGx tests vary widely. Key findings include:
- A review of policies from major commercial payers found that single-gene PGx tests are covered approximately 45% of the time they are mentioned in medical policies.
- Coverage determinations often depend on the specific gene-drug pair, with tests for HLA-B*57:01 prior to abacavir and HLA-B*15:02 prior to carbamazepine having the most consistent coverage across payers.
- Many commercial payers have more restrictive policies for multi-gene panels, often requiring specific diagnoses or prior treatment failures to establish medical necessity.
- Insurance coverage policies are evolving, with some commercial payers beginning to adopt more comprehensive approaches similar to recent Medicare policy changes.
The variability in coverage for PGx tests underscores the need for healthcare providers and laboratories to stay informed about the specific policies of major commercial payers in the United States. As the landscape continues to evolve, understanding these policies will be crucial for successful reimbursement.
Factors Affecting PGx Test Reimbursement
Reimbursement rates for PGx tests vary significantly based on the test type and clinical indication. The type of PGx test ordered plays a crucial role in determining reimbursement success. Recent data has shown that multi-gene panels have substantially higher reimbursement rates compared to single-gene tests.
Test Type: Single Gene vs. Panel Testing
The distinction between single-gene tests and panel testing is critical in understanding PGx test reimbursement. Studies have indicated that PGx panels were reimbursed at a significantly higher rate than single-gene tests (74% vs. 43%, p
The reimbursement advantage of panels varies by clinical indication. For instance, panels ordered for pain management and psychiatric conditions have particularly high success rates, with reimbursement rates of 78% and other conditions, respectively. On the other hand, targeted single-gene tests, such as CYP2D6 testing for pain management, have excellent reimbursement rates at 83%.
- The type of PGx test ordered significantly impacts reimbursement success, with multi-gene panels showing substantially higher reimbursement rates (74%) compared to single-gene tests (43%).
- The reimbursement advantage of panels varies by clinical indication, with particularly high success rates for panels ordered for pain management (78%) and psychiatric conditions.
- For certain specific indications, targeted single-gene tests may still have excellent reimbursement rates, such as CYP2D6 testing for pain management (83%).
- When selecting between single-gene and panel testing, providers should consider both the clinical indication and the specific payer policies to optimize reimbursement potential.
As the landscape of PGx testing continues to evolve, understanding the factors that influence reimbursement will be crucial for healthcare providers and laboratories to navigate the complex reimbursement process effectively.
Factors Affecting PGx Test Reimbursement
The reimbursement landscape for Pharmacogenomic (PGx) testing is significantly influenced by various factors, including diagnosis codes. Understanding these factors is crucial for providers and labs to navigate the complex reimbursement process successfully.
Diagnosis Codes and Their Impact
Diagnosis codes play a critical role in determining the reimbursement rate for PGx tests. The data indicates that claims submitted with multiple diagnosis codes have substantially higher approval rates compared to those with a single diagnosis code.
For instance, the reimbursement rate for claims submitted with three diagnosis codes was significantly greater than for claims submitted with a single diagnosis code (60% vs. 43%, p
The number of unique diagnosis categories also matters, with two unique diagnosis categories achieving a 63% reimbursement rate versus 44% for a single category. This suggests that not only the number but also the variety of diagnosis codes can impact reimbursement.
| Number of Diagnosis Codes | Reimbursement Rate |
|---|---|
| Single | 43% |
| Two | 63% |
| Three | 60% |
For single-gene tests, the strategic use of multiple relevant diagnosis codes is particularly important, as these tests show the greatest improvement in reimbursement rates with additional diagnostic justification. On the other hand, panel tests maintain relatively high reimbursement rates regardless of the number of diagnosis codes, though there is still a trend toward better outcomes with multiple unique diagnoses.
In conclusion, diagnosis codes significantly impact PGx test reimbursement. Providers and labs should ensure that they use multiple relevant diagnosis codes when submitting claims to maximize their reimbursement rates.
Factors Affecting PGx Test Reimbursement
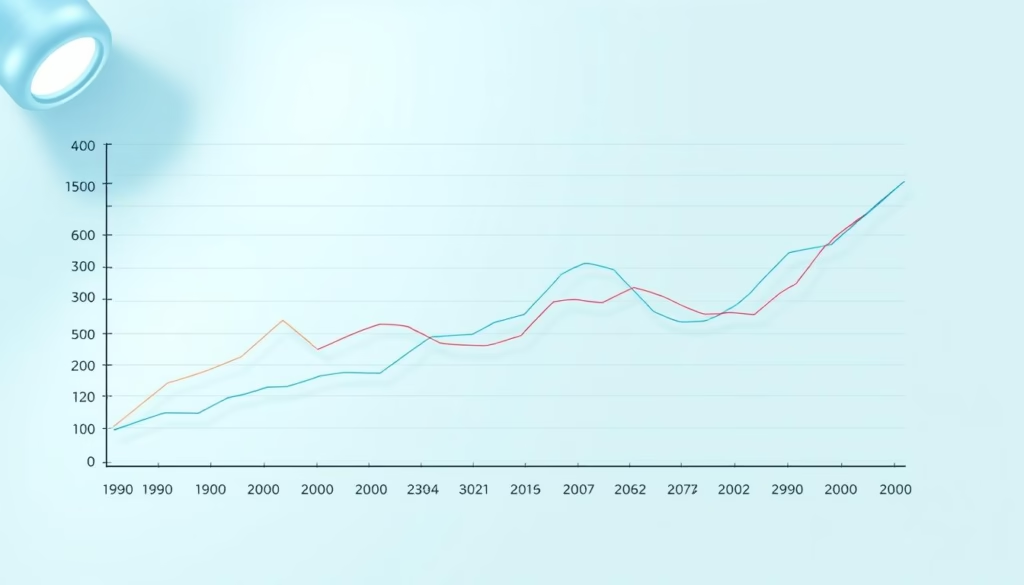
The reimbursement landscape for PGx testing is characterized by year-to-year variations in coverage. A retrospective analysis of claims data reveals significant fluctuations in reimbursement rates between 2019 and 2021.
Claims submitted in 2019 had the highest reimbursement rate at 63%, compared to 43% in 2020 and 44% in 2021. The number of claims increased over time, from 147 in 2019 to 249 in 2020, and 643 in 2021. This trend indicates growing clinical adoption despite reimbursement challenges.
Year-to-Year Variations in Coverage
Different payer types show distinct temporal trends. For instance, Medicare reimbursement rates rebounded significantly in 2021 (+13%), while Medicaid continued to decline (-18%). The timing of claim submission relative to policy updates can significantly impact reimbursement success.
- A notable decline in reimbursement rates was observed from 2019 (63%) to 2020 (43%), suggesting that policy changes rather than evidence evaluation drove coverage decisions.
- The reimbursement rate for commercial payers and Medicare increased in 2021 (+1% and +13%, respectively), but Medicaid and other payers continued to trend downward (−18% and −23%, respectively).
- The increasing volume of claims over time indicates strong provider belief in the value of PGx testing despite reimbursement challenges.
As stated by a recent study, “The variability in reimbursement rates for PGx testing highlights the need for providers and labs to stay current with payer policy changes.“
In conclusion, understanding the factors that affect PGx test reimbursement, including year-to-year variations in coverage, is crucial for providers and labs to navigate the complex reimbursement landscape.
Diagnosis-Specific Reimbursement Patterns
Pharmacogenomic testing for cardiology-related claims has shown varied reimbursement patterns, highlighting the need for a closer look at the current landscape. The data indicates that the majority of cardiology-related claims are for single-gene CYP2C19 tests, which are primarily used to guide antiplatelet therapy with clopidogrel.
Cardiology-Related Claims
Cardiology-related claims for pharmacogenomic testing predominantly involve CYP2C19 testing, making up 98% of the claims. Despite the FDA’s boxed warning for clopidogrel regarding CYP2C19 poor metabolizers, the reimbursement rate for these tests remains moderate at 52%. The data is as follows:
| Test Type | Number of Claims | Reimbursement Rate |
|---|---|---|
| Single-gene CYP2C19 | 275/281 (98%) | 52% |
| Panels | 4 (1%) | 100% |
| CYP2D6 | 2 (1%) | 0% |
The reimbursement rate for cardiology indications has not substantially improved over time, despite increasing evidence and guideline support. This suggests that payer policies are entrenched. Notably, when multi-gene panels are ordered for cardiology indications, they show excellent reimbursement rates (100% in limited samples), although they represent only a small fraction of cardiology-related testing.
Optimal diagnosis codes for cardiology claims include specific codes for acute coronary syndrome, coronary artery disease with stent placement, and cerebrovascular disease when clinically appropriate. Ensuring the correct use of these codes can improve reimbursement success.
Understanding the nuances of reimbursement for pharmacogenomic testing in cardiology can help providers and labs navigate the complex landscape more effectively. By focusing on the right testing types and diagnosis codes, they can improve their chances of successful reimbursement.
Diagnosis-Specific Reimbursement Patterns
Pharmacogenomic testing has become increasingly important in psychiatric care, with nearly half of all claims submitted relating to psychiatric diagnoses. This highlights the growing reliance on pharmacogenomic testing to guide treatment decisions in psychiatry.
Psychiatric Diagnosis Claims
The tests performed for psychiatric claims were most frequently CYP2D6 (43%), CYP2C19 (40%), and panel tests (17%). Notably, multi-gene panels for psychiatric indications show substantially higher reimbursement rates (72%) compared to single-gene tests for CYP2D6 (42%) or CYP2C19 (40%).
The higher reimbursement rate for panels in psychiatric care likely reflects the complex medication regimens often used in this specialty and the relevance of multiple genes. To optimize reimbursement, it is essential to use accurate diagnosis coding and documentation.
- Psychiatric diagnoses represent the largest category of pharmacogenomic testing claims.
- Testing for psychiatric indications typically involves CYP2D6 and CYP2C19.
- Multi-gene panels show higher reimbursement rates compared to single-gene tests.
- Optimal diagnosis coding should include specific mood disorder diagnoses and documentation of previous medication failures or adverse effects.
Key Considerations for Psychiatric Claims
To ensure successful reimbursement, providers and labs should focus on accurate diagnosis coding and thorough documentation. This includes using specific diagnosis codes for mood disorders and documenting any previous medication failures or adverse effects.
Diagnosis-Specific Reimbursement Patterns
Pharmacogenomic testing for pain management has emerged as a critical application with significant reimbursement success. The data indicates that claims submitted with a diagnosis code related to pain were reimbursed most often, at a rate of 72%. This is significantly higher than other common indications such as cardiology, psychiatry, and gastroenterology.
Pain Management Claims
Pain management represents the clinical indication with the highest overall reimbursement rate for PGx testing. For pain management, CYP2D6 single-gene testing shows the highest reimbursement success at 83%, reflecting its well-established role in opioid metabolism. Multi-gene panels are the most commonly ordered test type for pain management indications, accounting for 64% of pain-related claims, and maintain excellent reimbursement rates at 78%.
The strong reimbursement performance for pain-related testing likely reflects the growing recognition of the clinical utility of PGx in reducing adverse events and improving efficacy in pain management. To optimize reimbursement, diagnosis coding for pain management claims should include specific chronic pain diagnoses rather than symptom codes. Additionally, documenting failed medication trials when applicable can further support reimbursement claims.
- Pain management is the clinical indication with the highest reimbursement rate for PGx testing at 72%.
- CYP2D6 single-gene testing has the highest reimbursement success rate at 83%.
- Multi-gene panels are the most commonly ordered test type for pain management indications.
- Optimal diagnosis coding practices can enhance reimbursement success.
By understanding these trends and optimizing their practices, healthcare providers and laboratories can improve their reimbursement success for PGx tests related to pain management.
Diagnosis-Specific Reimbursement Patterns
Reimbursement for pharmacogenetic tests in gastroenterology varies significantly. This variability is influenced by several factors, including the type of test performed and the diagnosis codes submitted.
Gastroenterology-Related Claims
Gastroenterology-related claims for pharmacogenetic tests are primarily for CYP2C19 testing, which accounts for approximately 90% of GI claims. These tests are often used to guide proton pump inhibitor (PPI) therapy.
- CYP2C19 testing is the most common pharmacogenetic test in gastroenterology, with a reimbursement rate of 41%.
- Multi-gene panels, although less common (10% of GI claims), have a substantially higher reimbursement rate of 76%.
- The disparity between single-gene and panel reimbursement rates suggests that payers recognize the value of comprehensive genetic assessment.
To optimize reimbursement, it is crucial to submit the correct diagnosis codes. Specific diagnoses such as refractory GERD, Barrett’s esophagus, or H. pylori infection are preferred over general GI symptoms.
| Test Type | Reimbursement Rate | Frequency |
|---|---|---|
| CYP2C19 | 41% | 90% |
| Multi-gene Panels | 76% | 10% |
The data highlights the importance of choosing the right testing strategy and diagnosis codes to maximize reimbursement for pharmacogenetic tests in gastroenterology.
Payer-Specific Reimbursement Trends
Understanding the nuances of payer-specific reimbursement trends is essential for providers and labs navigating the complex world of pharmacogenomic (PGx) testing. The reimbursement landscape for PGx testing varies significantly across different payers, impacting the accessibility of these tests.
In the United States, Medicare reimbursement for PGx testing has evolved significantly, with a major policy shift occurring in 2020 when Medicare Administrative Contractors (MACs) began implementing more comprehensive coverage. The Molecular Diagnostic Services (MolDX) Program has established coverage for numerous PGx tests, with policies that heavily reference CPIC guidelines and FDA recommendations.
Medicare Reimbursement Patterns
Medicare reimbursement rates showed a notable pattern of decline from 2019 to 2020, followed by a significant rebound in 2021 (+13%), likely reflecting the implementation of new medical policy. Geographic variations in Medicare coverage exist based on which MAC serves a particular region, with MolDX-affiliated MACs generally providing the most comprehensive coverage. The year a claim is submitted to Medicare can significantly impact reimbursement success, with policies becoming increasingly favorable for PGx testing in recent years.
- Medicare reimbursement for PGx testing in the United States has evolved significantly.
- The Molecular Diagnostic Services (MolDX) Program has established coverage for numerous PGx tests.
- Geographic variations in Medicare coverage exist based on which MAC serves a particular region.
As payers continue to refine their reimbursement policies, it is crucial for stakeholders to stay informed about the latest developments in PGx testing coverage. By understanding these trends, providers and labs can better navigate the complex reimbursement landscape and optimize their billing practices for PGx tests.
Payer-Specific Reimbursement Trends
Commercial insurance trends for pharmacogenomic (PGx) testing reveal a complex landscape of coverage and reimbursement policies across the United States. As PGx testing becomes more prevalent, understanding these trends is crucial for providers and labs seeking reimbursement.
Commercial Insurance Trends
Commercial insurance coverage for PGx testing varies significantly across the country, with major national insurers having markedly different medical policies. Analysis of commercial payer policies shows that single-gene PGx tests are covered approximately 45% of the time they are mentioned in medical policies, though actual reimbursement rates may differ.
- Commercial payers typically have more restrictive coverage criteria for multi-gene panels compared to Medicare, often requiring specific diagnoses or prior treatment failures.
- Many commercial insurers delegate coverage decisions for molecular diagnostics to laboratory benefit managers (LBMs), adding another layer of complexity to the reimbursement process.
- Commercial insurance reimbursement rates for PGx testing showed a significant decline from 2019 to 2020, with only a modest recovery (+1%) in 2021, suggesting more conservative coverage trends.
The variability in coverage and reimbursement rates among commercial payers underscores the need for providers and labs to stay informed about the specific policies of the payers they work with. A detailed understanding of these trends can help in navigating the complex reimbursement landscape for PGx testing.
| Payer | Coverage Criteria | Reimbursement Rate |
|---|---|---|
| UnitedHealthcare | Specific diagnoses or prior treatment failures | 40% |
| Aetna | Multi-gene panels require prior authorization | 45% |
| Cigna | Single-gene tests covered for specific indications | 50% |
Payer-Specific Reimbursement Trends
The reimbursement landscape for pharmacogenomic testing varies significantly across different payer types. While some payers have shown an increase in reimbursement rates, others have trended downward, creating a complex environment for providers and labs.
Medicaid and Other Payers
Medicaid coverage for pharmacogenomic testing shows the most concerning trend among payer types, with reimbursement rates declining significantly from 2019 to 2021 (-18%). State Medicaid programs have considerable autonomy in coverage decisions, resulting in a patchwork of policies across the United States with substantial geographic disparities.
Other payers, including TRICARE and the Veterans Administration, show similarly declining reimbursement trends (-23% from 2020 to 2021), creating challenges for providers serving these populations. The divergence between Medicare’s improving coverage and Medicaid’s declining coverage raises equity concerns, as Medicaid beneficiaries may have reduced access to pharmacogenomic testing.
- Providers serving Medicaid populations should be particularly attentive to state-specific prior authorization requirements.
- Patient assistance programs may be necessary for Medicaid beneficiaries to access pharmacogenomic testing.
- The variability in coverage policies across different payers and regions complicates the reimbursement process.
Understanding these payer-specific reimbursement trends is crucial for navigating the complex landscape of insurance coverage for pharmacogenomic testing. By staying informed about the latest developments in coverage and reimbursement policies, providers and labs can better serve their patients and manage their practices effectively.
Evidence Requirements for Coverage Determinations
Clinical practice guidelines play a crucial role in determining coverage for pharmacogenomic testing. These guidelines, developed by professional societies, provide a framework for clinicians to make informed decisions about the use of pharmacogenomic tests.
Clinical Practice Guidelines
Clinical practice guidelines represent the most influential evidence type for pharmacogenomic coverage determinations. According to recent data, society guidelines were cited 413 times across analyzed medical policies, with the Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines being particularly impactful, accounting for 271 citations.
The significance of these guidelines lies in their ability to provide a standardized framework for the application of pharmacogenomics in clinical practice. Other influential guideline sources include the National Comprehensive Cancer Network (NCCN) for oncology-related testing and the American Heart Association (AHA) for cardiovascular applications.
- Drug-gene pairs with established CPIC guidelines are significantly more likely to receive coverage compared to those without such guidelines.
- When appealing coverage denials, referencing relevant clinical practice guidelines should be a primary strategy, as they carry substantial weight in payer decision-making.
The use of clinical practice guidelines in coverage determinations underscores the importance of evidence-based medicine in pharmacogenomics. By following these guidelines, healthcare providers can ensure that pharmacogenomic testing is used effectively and efficiently, ultimately improving patient outcomes.
“The integration of pharmacogenomics into clinical practice is becoming increasingly important, and clinical practice guidelines are at the forefront of this effort.”
Evidence Requirements for Coverage Determinations
The FDA plays a crucial role in shaping coverage determinations for pharmacogenetic testing through its recommendations and labeling. Pharmacogenetic testing, a key component of precision medicine, requires robust evidence to support coverage decisions. The FDA’s guidelines and labeling information significantly influence these decisions, particularly for drug-gene pairs included in the FDA’s Table of Pharmacogenetic Associations.
FDA Recommendations and Labeling
FDA recommendations and drug labeling information are critical in determining coverage for pharmacogenetic testing. Gene-drug pairs with FDA boxed warnings regarding genetic interactions achieve the most consistent coverage across payers. For instance, abacavir/HLA-B*57:01 and carbamazepine/HLA-B*15:02 are examples where FDA labeling has led to consistent coverage.
| Drug-Gene Pair | FDA Labeling | Coverage Consistency |
|---|---|---|
| Abacavir/HLA-B*57:01 | Boxed Warning | High |
| Carbamazepine/HLA-B*15:02 | Boxed Warning | High |
| Other Gene-Drug Pairs | Various Labeling | Variable |
Despite the importance of FDA biomarker information in drug labels, the absence of specific testing mandates often results in inconsistent coverage policies. When documenting medical necessity for pharmacogenetic testing, referencing relevant FDA labeling information can strengthen reimbursement claims, particularly for drugs with explicit genetic testing recommendations.
To improve reimbursement success, providers and labs should be aware of the FDA’s Table of Pharmacogenetic Associations and the Clinical Pharmacogenetics Implementation Consortium guidelines. These resources provide critical evidence for coverage determinations and can inform the development of more consistent coverage policies.
Evidence Requirements for Coverage Determinations
Payers require compelling clinical utility evidence to justify coverage for pharmacogenetic testing. This evidence is critical in demonstrating that pharmacogenetic tests lead to improved patient outcomes, thereby justifying their use in clinical practice.
Clinical Utility Evidence
Clinical utility evidence is increasingly important for coverage determinations, though payers vary in their evidence thresholds. The types of studies cited in medical policies include randomized controlled trials (RCTs), prospective studies, retrospective association studies, systematic reviews, and meta-analyses.
The frequency of citations for these study types varies, with RCTs and prospective studies being more commonly referenced to justify non-coverage rather than coverage. This suggests that payers may apply different evidence standards when evaluating studies that support versus refute the utility of pharmacogenetic testing.
A review of the evidence types cited in coverage policies reveals that systematic reviews and meta-analyses are also commonly used, particularly for evaluating the strength of evidence across multiple studies. The relative infrequency of cost-effectiveness citations indicates that economic analyses currently play a limited role in coverage determinations.
| Study Type | Frequency of Citation | Commonly Used For |
|---|---|---|
| Randomized Controlled Trials (RCTs) | High | Justifying non-coverage |
| Prospective Studies | High | Justifying non-coverage |
| Systematic Reviews and Meta-Analyses | High | Evaluating strength of evidence |
| Cost-Effectiveness Studies | Low | Economic analyses |
The development of clear guidelines and the accumulation of robust evidence are essential for improving coverage for pharmacogenetic testing. As the field continues to evolve, it is likely that the role of cost-effectiveness studies and other forms of evidence will become more prominent in coverage determinations.
Case Study: Retrospective Analysis of PGx Claims
A comprehensive analysis of pharmacogenomic (PGx) testing claims provides valuable insights into reimbursement patterns and factors affecting payment success. This section presents a retrospective analysis of PGx testing claims submitted by UF Health Pathology Laboratories to third-party payers for outpatient, clinical PGx tests performed between January 1, 2019, and December 31, 2021.
Study Methodology and Data Collection
The study methodology involved reviewing 1,039 outpatient claims for PGx tests submitted to various payers over a three-year period. The data collected included critical elements such as date of service, diagnosis codes (up to three per claim), payer information, billed charges, and actual reimbursement amounts.
For multi-gene panels, which were typically billed using multiple CPT codes, claims were consolidated and treated as a single testing event for analysis purposes. This approach allowed for a more accurate assessment of reimbursement rates and patterns.
- The study focused specifically on routine clinical outpatient testing, excluding PGx tests funded through research, paid for in cash, performed for inpatients, or conducted by third-party laboratories.
- The analysis of claims data revealed important trends and challenges in the reimbursement process for PGx testing.
By examining the reimbursement patterns for PGx testing, healthcare providers and laboratories can better understand the factors that influence payment success and develop strategies to improve reimbursement rates.
Case Study: Retrospective Analysis of PGx Claims
A comprehensive analysis of pharmacogenomic (PGx) testing claims revealed crucial insights into reimbursement trends. The study examined a total of 1,039 outpatient claims for PGx testing, providing a detailed understanding of the current reimbursement landscape.
Key Findings on Reimbursement Rates
The retrospective analysis revealed an overall reimbursement rate of 46% for PGx testing claims, with significant variations based on multiple factors. The findings can be summarized as follows:
- Multi-gene panels demonstrated substantially higher reimbursement success (74%) compared to single-gene tests (43%).
- Reimbursement rates varied by clinical indication, with pain management claims having the highest success rate (72%), followed by cardiology (52%), psychiatry (46%), and gastroenterology (44%).
- The number of diagnosis codes submitted significantly impacted reimbursement, with three diagnosis codes achieving a 60% success rate compared to 43% for single diagnosis claims.
The data highlights the importance of test type and diagnosis codes in determining reimbursement success. The overall reimbursement rate ranged from 36% to 48% across payers, indicating variability in coverage policies.
| Test Type | Reimbursement Rate |
|---|---|
| Multi-gene panels | 74% |
| Single-gene tests | 43% |
Temporal trends showed declining reimbursement rates from 2019 (63%) to 2020-2021 (43-44%), despite increasing clinical evidence supporting PGx testing utility. This decline suggests that payer policies may be becoming more restrictive over time.
The study’s findings have important implications for providers and labs seeking to navigate the complex landscape of PGx testing reimbursement. By understanding the factors that influence reimbursement success, healthcare professionals can optimize their testing strategies and improve patient outcomes.
Case Study: Retrospective Analysis of PGx Claims
The variable nature of reimbursement for PGx testing necessitates a strategic approach to testing and billing practices. A retrospective analysis of PGx claims provides valuable insights into the factors influencing reimbursement success, ultimately informing clinical practice.
The study’s findings have significant implications for healthcare providers and laboratories. By understanding the factors that affect reimbursement, providers can optimize their testing and billing practices to improve patient care and reduce administrative burdens.
Implications for Clinical Practice
The analysis revealed several key implications for clinical practice. Firstly, the type of test ordered significantly impacts reimbursement rates. Multi-gene panels demonstrate substantially higher reimbursement rates compared to single-gene tests, making them a preferable choice when clinically appropriate.
Including multiple relevant diagnosis codes is also crucial for reimbursement success. Providers should ensure that they submit claims with multiple diagnosis codes from different diagnostic categories to improve reimbursement rates.
The year-to-year variations in coverage policies highlight the need for providers to stay current with payer policy updates. Regularly reviewing and adjusting testing and documentation practices can help mitigate the impact of these changes.
| Factor | Impact on Reimbursement |
|---|---|
| Test Type | Multi-gene panels have higher reimbursement rates |
| Diagnosis Codes | Multiple relevant codes improve reimbursement success |
| Year-to-Year Variations | Staying current with payer policy updates is crucial |
Ultimately, the substantial variability in reimbursement necessitates transparent discussions with patients about potential out-of-pocket costs before ordering PGx testing. By understanding these factors and adapting their practices accordingly, healthcare providers can optimize PGx testing reimbursement and improve patient care.
Strategies to Improve Reimbursement Success
Strategic diagnosis code selection is crucial for maximizing reimbursement success in PGx testing. The choice of diagnosis codes can significantly impact the likelihood of successful reimbursement, making it essential for healthcare providers to understand the optimal strategies for code selection.
Optimal Diagnosis Code Selection
The data clearly indicates that using multiple relevant diagnosis codes can significantly increase reimbursement rates for PGx tests. Specifically, the reimbursement rate for claims submitted with three diagnosis codes was 60%, compared to 43% for claims with a single diagnosis code.
- Using up to three diagnosis codes on PGx testing claims can increase reimbursement rates from 43% to 60%.
- Including diagnosis codes from different categories, such as combining a psychiatric diagnosis with a pain diagnosis, can further enhance reimbursement rates to 63%.
- Prioritizing specific disease codes over symptom codes is recommended, as more definitive diagnoses typically align better with medical necessity criteria.
- For certain gene-drug pairs, specific diagnosis code combinations have demonstrated higher success rates, such as using acute coronary syndrome codes for CYP2C19 testing.
The importance of strategic diagnosis code selection cannot be overstated. By choosing the most relevant and specific codes, healthcare providers can improve their chances of successful reimbursement.
| Number of Diagnosis Codes | Reimbursement Rate |
|---|---|
| 1 | 43% |
| 2 | 63% |
| 3 | 60% |
By understanding the impact of diagnosis code selection on reimbursement and implementing strategies to optimize code choice, healthcare providers can enhance their reimbursement success rates for PGx testing.
Strategies to Improve Reimbursement Success
Accurate and detailed documentation is essential for successful PGx test reimbursement. Healthcare providers must ensure that all necessary information is included in the test order and supporting clinical notes to justify the medical necessity of the test.
Documentation Best Practices
Thorough documentation is critical for PGx test reimbursement. Several key elements should be included in every test order and supporting clinical notes.
- Medical Necessity: Clearly establish the link between the patient’s diagnosis, current or planned medications, and the specific genes being tested.
- Clinical Relevance: Document previous adverse drug reactions, treatment failures, or specific risk factors that make the patient a candidate for PGx-guided therapy.
- Guideline References: Reference relevant clinical practice guidelines (especially CPIC guidelines) and FDA labeling information to strengthen the case for medical necessity.
- Multi-Gene Panels: For multi-gene panels, clearly document the clinical relevance of each included gene to the patient’s care.
By following these documentation best practices, healthcare providers can improve their chances of successful reimbursement for PGx tests. It’s also crucial to discuss the cost and affordability of PGx testing with each patient due to the highly variable nature of reimbursement.
| Documentation Element | Description | Importance |
|---|---|---|
| Medical Necessity | Link between diagnosis, medications, and genes tested | High |
| Clinical Relevance | Previous adverse reactions, treatment failures, risk factors | High |
| Guideline References | CPIC guidelines and FDA labeling information | Medium |
| Multi-Gene Panels | Clinical relevance of each included gene | High |
As the landscape of PGx testing continues to evolve, staying informed about the latest clinical guidelines and reimbursement policies is vital for healthcare providers and laboratories alike.
Strategies to Improve Reimbursement Success
To improve reimbursement success, understanding prior authorization approaches is vital. Prior authorization is increasingly required for pharmacogenomic testing, making effective navigation of this process essential for reimbursement success.
Prior Authorization Approaches
Begin by researching specific payer requirements for pharmacogenomic testing prior authorization, as these vary significantly across health plans and may include specific forms or documentation. When submitting prior authorization requests, include comprehensive clinical information that aligns with the payer’s medical policy criteria, emphasizing guideline-supported indications.
- Research payer-specific requirements for prior authorization.
- Include comprehensive clinical information in prior authorization requests.
- Justify the use of multi-gene panels when applicable.
- Request a peer-to-peer review if prior authorization is denied.
For multi-gene panels, be prepared to justify why a panel approach is more appropriate than sequential single-gene testing for the specific patient. If prior authorization is denied, request a peer-to-peer review with a medical director who has expertise in genetics or the relevant specialty area, as this approach often leads to overturned denials.
Health plan medical policies that align with CPIC and medical society clinical practice guidelines, FDA recommendations, and/or published evidence are a key factor in enabling patient access to testing. By understanding and effectively navigating prior authorization processes, providers and labs can improve their chances of successful reimbursement for pharmacogenomic tests.
Laboratory Benefit Managers and Their Role
Laboratory Benefit Managers (LBMs) are increasingly pivotal in determining coverage for pharmacogenomic (PGx) testing. As the complexity and volume of genetic tests grow, health plans are relying more heavily on LBMs to inform their coverage decisions.
LBMs evaluate the clinical validity and utility of laboratory tests, develop comprehensive medical policy, and manage utilization through prior authorization and step therapy protocols. Major LBMs include Avalon Healthcare Solutions, eviCore healthcare, and AIM Specialty Health (now Carelon Insights), each with distinct payers policies for PGx testing.
Understanding LBM Policies
LBM policies often have more detailed and specific criteria than health plan policies, requiring providers to understand both the health plan’s general approach and the LBM’s specific requirements for reimbursement. For instance, some LBMs like Avalon cover numerous drug-gene pairs and panels, while others maintain more restrictive approaches to PGx testing.
It is critical for providers to identify which LBM manages genetic testing for a particular patient’s insurance, as this determines the specific policy criteria that must be met for successful reimbursement. Working effectively with LBMs requires a nuanced understanding of their policies and how they intersect with those of payers.
By understanding LBM policies and their implications for PGx testing, providers can better navigate the complex landscape of insurance coverage and improve their chances of successful reimbursement.
Laboratory Benefit Managers and Their Role
As Laboratory Benefit Managers (LBMs) continue to play a crucial role in managing diagnostic tests, understanding their influence on pharmacogenomic (PGx) testing is essential. LBMs are increasingly being utilized by health plans to oversee the utilization and reimbursement of laboratory tests, including PGx testing.
The role of LBMs in PGx testing is multifaceted, involving the development of coverage policies, managing prior authorizations, and ensuring compliance with payer requirements. Their decisions can significantly impact the reimbursement landscape for PGx tests.
Working Effectively with LBMs
To navigate this complex landscape, providers and laboratories must develop effective strategies for working with LBMs. This includes establishing direct communication channels with key LBMs, staying updated on their policy changes, and tailoring prior authorization requests to meet their specific evidence requirements.
- Establish direct communication channels with key LBMs in your region to resolve claims issues and clarify policy requirements.
- Stay current with LBM policy updates, which may occur more frequently than health plan policy changes and can significantly impact reimbursement success.
- When submitting prior authorization requests to LBMs, tailor your documentation to their specific evidence requirements, which often differ from general health plan criteria.
- Consider engaging with LBMs during their policy development process through public comment periods or advisory board participation to advocate for evidence-based coverage of PGx testing.
By adopting these strategies, providers and laboratories can improve their chances of successful reimbursement for PGx tests. As the healthcare industry continues to evolve, the importance of LBMs in managing diagnostic tests, including PGx testing, is expected to grow, making it crucial to maintain a proactive and collaborative approach.
Given the increasing volume and complexity of diagnostic tests, it is expected that more health plans will utilize LBMs. Therefore, understanding how to work effectively with LBMs is crucial for ensuring coverage and reimbursement for PGx tests.
Cost-Effectiveness of PGx Testing
Pharmacogenomic (PGx) testing is increasingly recognized for its potential to improve patient outcomes and reduce healthcare costs. As the healthcare industry continues to evolve, the economic benefits of PGx testing have become a significant area of interest.
A growing body of evidence supports the economic benefits of PGx testing, with approximately 75% of cost studies demonstrating that testing is either cost-effective or cost-saving compared to standard care. Economic analyses show that PGx testing can reduce overall healthcare costs by preventing adverse drug reactions, avoiding ineffective treatments, and reducing hospitalizations.
Evidence for Economic Benefits
The evidence for the economic benefits of PGx testing is compelling. An evaluation of 108 cost studies comparing PGx-guided therapy vs standard of care for drugs with CPIC guidelines found that roughly three-quarters of all studies determined PGx testing was cost-effective or cost saving. The cost-effectiveness of pharmacogenetic tests varies by clinical scenario, with particularly strong evidence for certain applications such as HLA testing before abacavir treatment and CYP2C19 testing before clopidogrel therapy.
For more information on PGx testing, you can refer to our comprehensive guide on what to look for in pharmacogenomics testing kits in.
- The economic case for multi-gene panel testing is particularly strong, as the incremental cost of testing additional genes is minimal compared to the potential benefits of comprehensive medication guidance.
- Despite compelling economic evidence, cost-effectiveness studies are infrequently cited in payer coverage policies, suggesting an opportunity to better incorporate this information.
Cost-Effectiveness of PGx Testing
Effectively communicating the value of PGx testing to payers is crucial for expanding coverage and ensuring equitable access to these important diagnostic tools. As the healthcare landscape continues to evolve, it is essential to demonstrate the clinical utility and economic benefits of PGx testing.
The cost-effectiveness of PGx testing is a critical factor in determining reimbursement policies. To achieve favorable coverage decisions, it is necessary to present robust evidence that supports the value of PGx testing in improving patient outcomes and reducing healthcare costs.
Communicating Value to Payers
When engaging with payers, focus on both clinical utility evidence and economic analyses that demonstrate cost-effectiveness or cost savings relevant to their specific population. Key strategies include:
- Highlighting the downstream cost implications of PGx testing, such as reduced hospitalizations for adverse drug reactions and decreased medication wastage.
- Developing case studies specific to the payer’s population that illustrate the real-world economic and clinical benefits of pharmacogenetic tests in practice.
- Collaborating with professional societies and patient advocacy groups to present a unified message about the value of PGx testing and the importance of consistent coverage policies.
By adopting these strategies, stakeholders can effectively communicate the value of PGx testing to payers, ultimately expanding coverage and improving patient access to these critical diagnostic tools. For more information on the benefits of PGx testing, refer to studies such as those published on PMC.
Regulatory and Policy Developments
The regulatory landscape for pharmacogenomic (PGx) testing has undergone significant changes in recent years. Several policy developments have expanded coverage and improved equitable access to PGx testing.
One of the key advancements is in Medicare coverage. Since 2020, Medicare Administrative Contractors (MACs) have begun implementing policies that comprehensively cover PGx testing. By December 2021, all but one MAC had approved comprehensive coverage for PGx testing, thereby increasing accessibility for over 48 million Medicare beneficiaries.
Recent Policy Changes
State-level legislation has also played a crucial role in mandating coverage for biomarker testing, including pharmacogenetic markers. Illinois, Arizona, and Rhode Island have enacted such legislation, setting important precedents for other states.
- Professional societies have updated guidelines to more explicitly recommend PGx testing for specific scenarios, thereby strengthening the evidence base for coverage determinations.
- The FDA has continued to update drug labeling with pharmacogenetic information, including the Table of Pharmacogenetic Associations, which categorizes drug-gene interactions based on evidence strength.
These developments underscore the evolving nature of PGx testing and its integration into clinical practice. As guidelines continue to be refined and managed care policies adapt, the accessibility and utility of PGx testing are likely to expand further.
| State | Legislation Status | Impact on PGx Testing |
|---|---|---|
| Illinois | Enacted | Mandatory coverage for biomarker testing |
| Arizona | Enacted | Mandatory coverage for biomarker testing |
| Rhode Island | Enacted | Mandatory coverage for biomarker testing |
Regulatory and Policy Developments
As state laws evolve, they are having a profound impact on the coverage of pharmacogenomic testing. Recent legislation in several states has mandated coverage for biomarker testing, including pharmacogenetic markers that predict medication response.
State-Level Legislation
State-level legislation is emerging as a powerful force in expanding access to pharmacogenomic testing. Several states have enacted laws that require insurance coverage for biomarker testing, including Illinois, Arizona, and Rhode Island. These laws apply to both commercial insurance plans and state Medicaid programs, creating a more consistent coverage environment within these states.
The impact of these laws is significant, as they override more restrictive managed care policies. For instance, a table comparing the coverage policies before and after the legislation in these states highlights the changes:
| State | Pre-Legislation Coverage | Post-Legislation Coverage |
|---|---|---|
| Illinois | Limited coverage for PGx testing | Mandatory coverage for biomarker testing |
| Arizona | Variable coverage depending on the payer | Comprehensive coverage for PGx testing |
| Rhode Island | Restricted coverage for certain tests | Expanded coverage for pharmacogenetic markers |
Advocacy organizations, such as the American Cancer Society’s Cancer Action Network, are actively working to expand similar legislation to additional states. Providers and laboratories should monitor state-specific legislation, as these laws may create coverage opportunities that override more restrictive managed care policies.
- State laws are increasingly influencing pharmacogenomic testing coverage.
- Illinois, Arizona, and Rhode Island have passed legislation mandating coverage for biomarker testing.
- These laws create a more consistent coverage environment and may override restrictive managed care policies.
Challenges in PGx Test Reimbursement
The variability in coverage for PGx tests represents a substantial challenge for both providers and laboratories seeking reimbursement. This issue is at the forefront of concerns in the field of pharmacogenomics.
A significant analysis of major US health insurers revealed dramatic differences in coverage policies, with some policies covering all 65 clinically relevant drug-gene pairs while others covered fewer than 10. This inconsistency creates a significant administrative burden for providers and laboratories, who must navigate different requirements for each payer.
Variability in Coverage Policies
The extreme variability in coverage policies across payers is one of the most significant challenges in PGx test reimbursement. For instance, Molecular Diagnostic Services, which determines whether a molecular diagnostic test is covered by Medicare, covered pharmacogenetic testing for all 65 clinically relevant drug-gene pairs evaluated. In contrast, 8 of the 12 policies reviewed covered 10 or fewer drug-gene pairs.
- The inconsistency in coverage creates significant administrative challenges for providers and laboratories.
- The variability extends beyond which tests are covered to include differences in documentation requirements, prior authorization processes, and evidence standards.
- This patchwork of coverage policies creates geographic and socioeconomic disparities in access to PGx testing, as patients’ ability to benefit from testing depends heavily on their insurance coverage and the specific managed care policies in place.
The impact of these disparities underscores the need for more uniform medical policy determinations across payers. By addressing the variability in coverage policies, the healthcare industry can work towards improving access to PGx testing and enhancing patient outcomes.
Challenges in PGx Test Reimbursement
One of the major challenges in PGx test reimbursement is the inconsistency in how evidence is assessed by different payers. The subjective interpretation of scientific studies leads to varying coverage determinations, creating an uncertain environment for test developers and laboratories.
Evidence Threshold Disparities
Significant disparities exist in how payers evaluate and apply evidence when making coverage determinations for pharmacogenetic testing. The same scientific studies are sometimes cited to support opposite coverage decisions by different payers, highlighting the subjective nature of evidence interpretation.
- Clinical practice guidelines, particularly CPIC guidelines, are frequently cited across policies, but payers vary in how they weigh these recommendations against other evidence types.
- Randomized controlled trials are often considered the gold standard for evidence, yet their application to PGx testing is inconsistent, with some payers requiring trial data specific to each gene-drug pair.
- These disparities create a challenging environment for test developers and laboratories seeking to generate sufficient evidence for broad coverage of PGx testing.
The variability in evidence thresholds and interpretation of guidelines complicates the reimbursement process for PGx tests, making it essential for stakeholders to understand these challenges to navigate the complex landscape effectively.
Challenges in PGx Test Reimbursement
The reimbursement landscape for PGx testing is characterized by a significant administrative burden. This burden affects healthcare providers and laboratories, making it challenging to incorporate PGx testing into routine care.
Administrative Burden
The administrative burden associated with PGx test reimbursement creates significant challenges. Prior authorization requirements for PGx testing have increased substantially, with many payers implementing complex documentation requirements that consume valuable clinical time.
- Increased Administrative Complexity: The variability in coverage policies necessitates payer-specific workflows, increasing administrative complexity and costs for healthcare organizations.
- Claims Denials: Claims denials for PGx testing are common, requiring extensive appeals processes that further increase administrative costs and delay patient care.
- Impact on Smaller Practices: This administrative burden disproportionately impacts smaller practices and laboratories with limited resources, potentially exacerbating disparities in access to PGx testing.
Without health plan coverage, patients who are not offered testing due to provider concerns about coverage or who are unable to pay out of pocket may miss out on the benefits of molecular diagnostics, potentially resulting in suboptimal treatment. The benefits of PGx testing outweigh the costs, making it essential to address these reimbursement challenges.
By understanding the administrative burden associated with PGx test reimbursement, healthcare providers and laboratories can better navigate the complexities of insurance coverage and billing codes, ultimately improving patient access to these critical tests.
Future Outlook for PGx Reimbursement
As we look to the future, the landscape of PGx reimbursement is poised for significant changes. The current state of insurance coverage and billing codes for PGx tests is complex, but there are promising signs of improvement.
Medicare’s expanded coverage policies are likely to influence commercial payers, potentially leading to more consistent coverage across the insurance landscape. Additionally, state-level legislation mandating biomarker testing coverage will continue to expand, creating important precedents and reducing geographic disparities in access.
Ongoing research demonstrating both clinical utility and cost-effectiveness of PGx testing will strengthen the evidence base for coverage determinations. Collaborative efforts between the PGx community, professional societies, and payers to standardize evidence evaluation could lead to more consistent coverage policies.
The continued evolution of clinical practice guidelines will further clarify appropriate testing scenarios, potentially reducing variability in coverage determinations. As technology advances and costs decrease, the economic case for comprehensive PGx testing will become increasingly compelling to payers focused on value-based care.
In conclusion, while significant challenges remain, the future outlook for PGx reimbursement is promising. Providers and laboratories should continue to develop strategies for navigating the complex reimbursement landscape while advocating for more rational, evidence-based coverage policies guided by evolving guidelines and research findings presented in this article.
By doing so, we can improve patient access to PGx tests that meet evidence requirements, ultimately enhancing the quality of care through personalized medicine approaches as discussed in this article, and supported by emerging guidelines.