The Institute of Medicine reveals that one-third of the U.S. population grapples with persistent pain, underscoring a critical public health issue that necessitates novel solutions1. Chronic pain not only diminishes life quality but also escalates the reliance on pharmaceuticals, notably opioids, with one in five patients receiving a prescription1. Alas, these medications often fall short; up to one-third of patients on prolonged opioid therapy for nonmalignant chronic pain report ineffectiveness or poor tolerance of their treatment1.
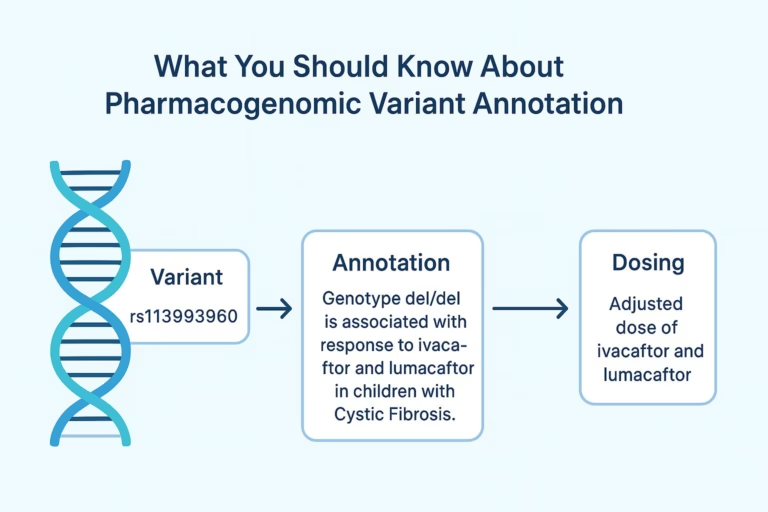
Pharmacogenomics heralds a transformative shift, moving from the traditional trial-and-error medication approach to a more precise and effective strategy. This discipline utilizes genetic profiles to forecast individual drug responses, allowing healthcare providers to customize pain management strategies effectively. Notably, variants in the CYP450 enzyme, particularly CYP2D6, significantly influence the metabolism of opioids such as codeine and tramadol1.
Given that over 90% of the population possesses genetic variations affecting medication response, the integration of pharmacogenomics into clinical practices could significantly improve patient outcomes and enhance pain relief1. Moreover, the CPIC and the Dutch Pharmacogenetics Working Group have evaluated over 100 gene-drug pairs for pharmacogenomic guidance, emphasizing the imperative for sustained pharmacogenomics research in pain management1. Let’s dive into clinical validity of pharmacogenomics in pain management.

Understanding Pharmacogenomics
Pharmacogenomics is a groundbreaking field that delves into the genetic variations influencing drug responses, especially in pain management. It’s crucial for the development of precision medicine for pain treatment, which customizes therapies according to individual genetic makeup. For example, CYP2D6 polymorphisms significantly affect the efficacy and safety of pain medications like codeine and tramadol2.
Genetic variations can modify drug metabolism, classifying patients as poor, intermediate, or ultrarapid metabolizers. Poor metabolizers often experience lower serum morphine levels from codeine, necessitating treatment adjustments2. Furthermore, the Clinical Pharmacogenetics Implementation Consortium (CPIC) has established guidelines for selecting opioids based on genetic profiles3.
The adoption of pharmacogenomic tests signals a shift towards personalized pain management. With over 250 medications linked to pharmacogenomic testing in FDA-approved labels, the trend towards tailored treatment is evident4.
As pharmacogenomic testing becomes more prevalent, grasping its underlying principles can refine pain management strategies. Genetic analysis in treatment plans can lead to better therapeutic outcomes and reduced adverse drug reactions. It’s vital for healthcare professionals and patients to comprehend pharmacogenomics to enhance pain management and improve overall care.
Current Trends in Pain Management
The landscape of pain management is undergoing a significant transformation, gravitating towards more personalized care modalities. This shift is a direct response to the escalating opioid crisis, which necessitated a public health emergency declaration by the Health and Human Services in 20175. Healthcare professionals now advocate for a multifaceted approach, combining pharmacological and non-pharmacological interventions. This strategy not only improves treatment efficacy but also underscores the importance of individualized care.
Pharmacogenomic testing has emerged as a pivotal tool, enabling the prediction of patient responses to various pain medications. Chronic pain affects a staggering one in three Americans6, underscoring the necessity for tailored therapeutic interventions. Genomic testing in pain therapy facilitates the optimization of drug regimens, thereby minimizing adverse effects and enhancing treatment outcomes.
The adoption of clinical pharmacogenomic testing is accelerating, aimed at synchronizing treatment with individual genetic profiles. This approach ensures healthcare providers can tailor medicine to patients’ genetic predispositions, environmental factors, and lifestyle7. The integration of this testing into clinical practice is expected to lead to improved patient outcomes and optimize the efficacy of pain management therapies.
| Trend | Description | Impact |
|---|---|---|
| Reduced Opioid Reliance | Shift towards alternative pain management strategies | Lower incidence of addiction and overdose |
| Multimodal Approaches | Combination of pharmacotherapy and non-pharmacological methods | Improved overall treatment outcomes |
| Pharmacogenomic Testing | Personalized medicine based on genetic profiles | Enhanced efficacy and reduced adverse effects from pain medications |
The Role of Genetic Variations in Drug Response
Grasping the intricacies of genetic variations in drug response is paramount for refining pain management protocols. Genomic variants, especially those influencing cytochrome P450 enzymes, substantially shape the metabolism of analgesics, impacting their efficacy and safety profiles.
It is noteworthy that 90% of medications, including analgesics, rely on CYP450 enzymes for their metabolism, underscoring the significance of pharmacogenomic markers for pain relief in clinical practice8. Genetic differences in these enzymes can classify individuals into poor, intermediate, extensive, or ultra-rapid metabolizers, a classification pivotal for predicting drug efficacy.
Pharmacogenetic testing enables healthcare professionals to discern these genetic variations, thus enabling the formulation of personalized treatment regimens. Such an approach not only optimizes therapeutic dosages but also mitigates adverse reactions, leading to reduced opioid use and diminished post-operative pain in patients8.
Identifying specific single-nucleotide polymorphisms (SNPs) and allelic variants equips clinicians with the knowledge to tailor analgesic dosing. Given that approximately 65% of patients experience postoperative pain, pharmacogenetic insights are crucial for devising effective pain management strategies8.
Emerging pharmacogenomic research underscores the critical role of CYP2D6 phenotypes and allelic variants in optimizing therapeutic outcomes. For instance, the detection of CYP2D6*4 variants aids in determining analgesic dosages and reducing adverse drug reactions, thereby improving patient care9.
In conclusion, integrating genetic insights into pain management not only propels the field of pharmacogenomics but also marks a crucial advancement towards personalized medicine, particularly for those grappling with chronic pain.
Clinical Validity of Pharmacogenomics in Pain Management
The clinical validity of pharmacogenomics in pain management is increasingly recognized as vital for enhancing patient outcomes. Pharmacogenomic testing has the potential to predict individual medication responses based on genetic profiles, providing healthcare providers with the necessary insights to tailor pain management strategies effectively. A study aimed at evaluating patient experiences with pharmacogenomic-based individualized medicine in Jacksonville, FL, highlights the interest in this area10. Similarly, research conducted in Rochester, MN, investigates gene variation and response to medications like Naproxen in women with heavy menstrual bleeding, showcasing the clinical relevance of pharmacogenomics in specific populations10.
Overview of Clinical Validity
Clinical validity refers to the accuracy with which pharmacogenomic data can predict a patient’s response to specific medications. Understanding the impact of genetic variations can identify patients at risk of inadequate pain relief or adverse effects from opioid therapies, thus underscoring the importance of this field in pain management. In Rochester, MN, studies compare pharmacogenomic testing results across various companies, aiming to standardize practices and ensure reliable outcomes in medication choices10.
Evidence Supporting Pharmacogenomic Testing
Evidence supporting pharmacogenomic testing continues to grow, with numerous studies demonstrating its benefits. Among 146 patient pharmacogenomics reports analyzed, 57.5% exhibited moderate drug-gene interactions (DGI), while 5.5% indicated serious interactions11. Further, 65.8% of patients experienced at least one moderate DGI or drug-drug interaction (DDI), showcasing the crucial role of genetic insights in prescribing decisions11. In total, 85 patients altered their prescriptions based on pharmacogenomic reports, leading to improved therapeutic strategies11.
Benefits of Pharmacogenetic Testing for Pain Relief
Pharmacogenetic testing unveils a plethora of benefits that revolutionize pain management by tailoring treatment to individual genetic profiles. This modality elucidates whether a specific medication is likely to be efficacious for a particular patient, thereby refining pain therapy options12. Moreover, it evaluates the optimal dosage of a medication, predicated on genetic determinants, thereby diminishing the occurrence of ineffective treatments12.
The employment of pharmacogenomic markers for pain alleviation enables predictions regarding the propensity for severe side effects from certain medications. This is especially crucial when considering medications like opioids, which can exhibit significant adverse reactions13. The identification of gene variants through pharmacogenetic tests delineates how medications will impact individuals, facilitating the creation of bespoke treatment regimens12.
Pharmacogenetic findings indicating a medication’s unsuitability for a patient prompt healthcare providers to expedite the exploration of alternative treatments, eschewing the traditional trial-and-error methodology12. This targeted strategy not only augments patient satisfaction but also fosters adherence to treatment protocols, as patients exhibit a favorable response to medications congruent with their genetic makeup.
The burgeoning acceptance of precision medicine in pain treatment has led the clinical community to acknowledge the pivotal role of pharmacogenetic testing. For example, the Clinical Pharmacogenetics Implementation Consortium’s 2021 guidelines underscore the importance of genotype testing for opioid therapy, highlighting the significance of genetic predispositions in pain management13.
By amalgamating pharmacogenomic insights with conventional treatment paradigms, healthcare providers can make data-driven decisions that not only augment the efficacy of pain relief strategies but also bolster patient safety and experience. The minimal risks associated with pharmacogenetic testing, such as mild pain at the injection site, underscore its feasibility and acceptance in treatment planning12.
Challenges in Implementing Pharmacogenomics in Clinical Practice
The integration of pharmacogenomics into clinical practice is fraught with significant challenges. A major concern lies in the variability of laboratory practices and the *inconsistency* in insurance coverage for genomic testing in pain therapy. Approximately 10% of children receive one drug for which a change in prescribing due to genetic variants could be recommended14. Limited understanding and knowledge among clinicians regarding pharmacogenomic principles further complicate its application in pain management.
Research continues to unveil a plethora of data regarding gene-drug interactions. For example, CYP2C9 metabolizes approximately 25% of clinically administered drugs, with poor metabolizers prevalent in varying rates across populations; this includes 3-4% in Southern Europe, and less than 1% in Asian and African populations, except for Emiratis at 11.1%14. Additionally, the prevalence of CYP2C19 poor metabolizers stands at 2-5% among Caucasians and Africans, with a notable rise to around 15% in Asian populations14.
Despite the insights from pharmacogenomics research, translating this information into practical clinical utility faces ethical concerns and regulatory hurdles. The U.S. Food and Drug Administration (FDA) emphasizes the need for genomic data collection and the integration of genetic differences that can affect drug responses and therapeutic requirements15. Moreover, the complexities of managing multimorbidity and polypharmacy further complicate the implementation, as clinicians grapple with unique drug metabolism rates that can vary drastically—such as a more than sixfold difference in details of drug exposure to diazepam due to CYP2C19 genetic polymorphisms14.
Adverse drug reactions remain a critical issue in patient safety, contributing to 135,000 deaths annually in the USA alone, along with an economic burden surpassing USD 136 billion16. Addressing the challenges in implementing pharmacogenomics is essential to optimizing pain management strategies and improving patient outcomes.

Personalized Medicine in Pain Management
Personalized medicine in pain management represents a paradigm shift, offering a tailored approach to each patient’s unique needs. Through pharmacogenomics research, healthcare professionals can discern a treatment strategy that resonates with an individual’s genetic makeup. This methodical understanding of genetic profiles underpins the selection of precise medications, thereby enhancing the efficacy of pain treatment.
Studies underscore the importance of genetic factors in treatment outcomes, with 57.5% of patients exhibiting moderate drug interactions11. This statistic highlights the necessity of a shift from generic to individualized health strategies. Precision medicine for pain treatment is gaining traction, offering a more nuanced approach to alleviating suffering.
Moreover, the integration of pharmacogenomic testing has led to significant changes in prescription management, with 83.3% of patients benefiting from tailored treatment plans11. This precision not only optimizes therapeutic outcomes but also minimizes adverse reactions. By leveraging genetic insights, healthcare providers can pinpoint the most effective medications, ensuring targeted pain relief.
The Precision Medicine Initiative has catalyzed a new wave of projects aimed at refining personalized medicine. This initiative has sparked a dialogue on redefining disease taxonomy, advocating for a holistic approach to patient care17. Such endeavors signal a transformative shift in healthcare, placing the patient at the forefront of medical decision-making.
Pharmacogenomics is poised to revolutionize pain management, heralding a new epoch in healthcare. As research progresses and patient-centered strategies gain prominence, the future promises a radical reimagining of chronic pain treatment. This evolution will likely redefine how pain is diagnosed, managed, and understood, offering hope to those grappling with persistent discomfort.
| Description | Statistical Insight |
|---|---|
| Moderate drug interactions in patient reports | 57.5% |
| Serious pharmacogenomic interactions | 5.5% |
| Patients with moderate or serious interactions | 65.8% |
| Patients experiencing prescription changes | 83.3% |
Future Directions in Pharmacogenomics Research
The domain of pharmacogenomics is poised for substantial advancement, with a focus on the complex interplay between genetic variations and the efficacy of pain medications across varied populations. As research evolves, the anticipation grows for a deeper understanding of drug-gene interactions. This knowledge will underpin the development of clinical guidelines that seamlessly integrate pharmacogenomic testing into standard medical practices. Such a shift promises to empower healthcare professionals in tailoring therapeutic strategies, particularly in pain management, thereby improving patient outcomes.
Furthermore, the trajectory of pharmacogenomics research may expand beyond conventional opioid treatments to encompass a spectrum of non-opioid alternatives. This evolution is contingent upon technological and analytical innovations, which are expected to enhance pharmacogenomic endeavors. These advancements will facilitate the development of tailored treatment plans that resonate with individual genetic profiles, benefiting a wider patient demographic.
As healthcare systems increasingly adopt pharmacogenomic testing, the integration of these methodologies into clinical practice is set to diminish the risks associated with adverse drug reactions. This approach is poised to not only elevate patient care efficiency but also to significantly reduce healthcare costs. The exploration of these avenues promises a paradigm shift towards more personalized and effective pain management strategies, as underscored by recent research emphasizing the pivotal role of pharmacogenomics181920.
Source Links
- https://www.wolterskluwer.com/en/expert-insights/pharmacogenomics-effect-of-gene-variability-on-pain-management – Blog Post – Pharmacogenomics: Effect of Gene Variability on Pain Management
- https://www.uspharmacist.com/article/pharmacogenomic-considerations-in-opioid-therapy – Pharmacogenomic Considerations in Opioid Therapy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10020807/ – Evidence Regarding Pharmacogenetics in Pain Management and Cancer
- https://medicine.iu.edu/blogs/bioethics/dangerous-ignorance – Dangerous Ignorance: What Patients Don’t Understand about Pharmacogenomics
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8656342/ – Engaging pharmacogenomics in pain management and opioid selection
- https://www.degruyter.com/document/doi/10.1515/dmpt-2016-0005/html – Pharmacogenomics in pain treatment
- https://www.dovepress.com/understanding-the-psychological-physiological-and-genetic-factors-affe-peer-reviewed-fulltext-article-JPR – Genetic Factors Affecting Precision Pain Medicine | JPR
- https://www.mdpi.com/2227-9059/12/4/729 – Pharmacogenetic Approaches in Personalized Medicine for Postoperative Pain Management
- https://www.dovepress.com/the-pharmacogenomics-of-pain-management-prospects-for-personalized-med-peer-reviewed-fulltext-article-JPR – The pharmacogenomics of pain management: prospects for personalized me | JPR
- https://www.mayo.edu/research/clinical-trials/tests-procedures/pharmacogenomic-testing/ – Pharmacogenomic Testing Clinical Trials – Mayo Clinic Research
- https://xmed.jmir.org/2022/2/e32902 – Effects of Pharmacogenomic Testing in Clinical Pain Management: Retrospective Study
- https://medlineplus.gov/lab-tests/pharmacogenetic-tests/ – Pharmacogenetic Tests: MedlinePlus Medical Test
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10341655/ – Pharmacogenetic Guided Opioid Therapy Improves Chronic Pain Outcomes and Comorbid Mental Health: A Randomized, Double-Blind, Controlled Study
- https://www.mdpi.com/1424-8247/16/11/1596 – Impact of Pharmacogenomics in Clinical Practice
- https://www.fda.gov/files/drugs/published/Clinical-Pharmacogenomics–Premarket-Evaluation-in-Early-Phase-Clinical-Studies-and-Recommendations-for-Labeling.pdf – Clinical Pharmacogenomics: Premarket Evaluation in Early-Phase Clinical Studies and Recommendations for Labeling
- https://www.mdpi.com/2075-4426/11/5/394 – Implementing Pharmacogenomics Testing: Single Center Experience at Arkansas Children’s Hospital
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8517910/ – Understanding the Psychological, Physiological, and Genetic Factors Affecting Precision Pain Medicine: A Narrative Review
- https://medicine.stanford.edu/news/current-news/standard-news/minimizing-the-guessing-game-in-pain-management.html – Minimizing the Guessing Game in Pain Management
- https://www.fightcancer.org/releases/new-paper-finds-barriers-equitable-discovery-and-implementation-pharmacogenomic-testing – New Paper Finds Barriers to Equitable Discovery and Implementation of Pharmacogenomic Testing in Cancer Care Despite its Power to Improve Patient Outcomes
- https://www.ons.org/cjon/27/2/pharmacogenomic-germline-testing-applications-oncology-nursing – Pharmacogenomic Germline Testing: Applications in Oncology Nursing